Revolutionary Research: Cancer Insights Pave the Way for Breakthrough Alzheimer's Therapies
2024-09-18
Revolutionary Research: Cancer Insights Pave the Way for Breakthrough Alzheimer's Therapies
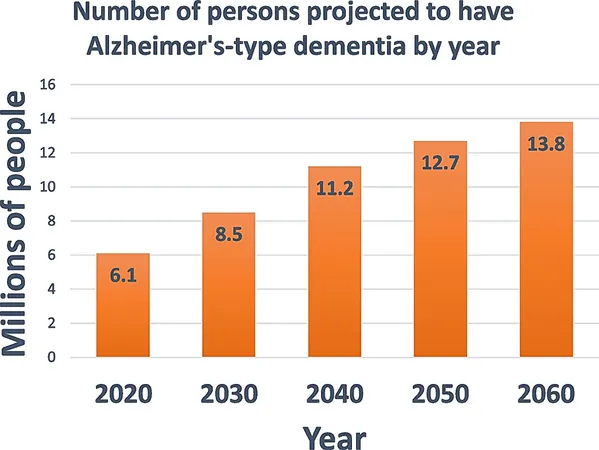
In a powerful convergence of medical disciplines, researchers at the University of Kentucky (UK) are leveraging critical insights from cancer research to revolutionize therapies for Alzheimer’s disease. As the conversation around Alzheimer's disease intensifies, particularly concerning disease-modifying therapies, clinicians find themselves grappling with significant uncertainties about their effectiveness, safety, and economic implications. The stage is set for a paradigm shift as experts call for a more aggressive approach to treating Alzheimer’s, similar to strategies employed in cancer care.
Leading this transformative work are Dr. Greg Jicha and Dr. Pete Nelson from UK’s Sanders-Brown Center on Aging, who recently published two groundbreaking papers that review the sharing of knowledge between the Alzheimer’s Disease Research Center and the UK Markey Cancer Center. These studies are more than mere academic contributions: they encapsulate the vital importance of interdisciplinary collaboration aimed at tackling age-related clinical syndromes that are becoming alarmingly prevalent.
The first publication in *Alzheimer's Research & Therapy* examines the striking parallels between dementia and cancer. Notably, cancer research has produced an impressive array of effective treatments, while advancements in dementia therapies have lagged, leaving many patients bereft of viable options. This new study strongly suggests that methodologies and experiences from cancer research could illuminate a path forward for Alzheimer’s treatments.
One key observation from the study is that in cancer care, patients who are untreated typically face an imminent risk of death, prompting healthcare providers to adopt more aggressive treatment protocols. Conversely, the Alzheimer’s research community has relied on a more cautious approach, often disenfranchising at-risk patients from participating in clinical trials that could benefit them.
Dr. Nelson encapsulates the ethical dilemma: "Dementia is a horrendous condition, carrying severe risks. It's ethical to let patients choose more aggressive therapies, provided they understand the implications."
The hesitation surrounding the adoption of novel Alzheimer’s therapies often arises from three pillars of concern: effectiveness in preventing cognitive decline, safety for patients, and high treatment costs. A second paper published in *Alzheimer's and Dementia: Translational Research and Clinical Interventions* addresses these barriers by comparing the anti-amyloid therapy, lecanemab, to biologic agents from oncology, including trastuzumab for breast cancer and bevacizumab for lung cancer. The results indicate that lecanemab offers comparable benefits and side effects, thereby positioning it within an acceptable context for wider clinical use.
Moreover, the emerging findings reveal that even participants in placebo groups frequently experience beneficial outcomes, stressing the untapped potential in clinical research participation. The authors advocate for borrowing critical strategies from cancer treatment, such as balancing side effects with the consequences of nontreatment and embracing combination therapies—a call to action for dementia researchers.
Dr. Jicha expressed his frustrations with the slow integration of Alzheimer’s research parallels from cancer treatments as he sees firsthand how oncology thrives on rapid assessments of treatment efficacy. "We believe by adopting this mindset, we can chart a clearer course forward for Alzheimer’s therapies," he said, emphasizing the urgency of the situation.
In oncology, the escalation of treatments is often driven by immediate needs; patients in critical stages require fast, actionable responses. However, with Alzheimer’s, the timeline is drastically different—the progression from initial symptoms to severe impairment can take years. Patients and their providers often hesitate, questioning if potential side effects of long-term treatment are truly worth the uncertainty of delayed benefits.
Dr. Susanne Arnold, also involved in this pioneering research, highlights the need for the medical community to adopt a long-term view in Alzheimer’s treatment: "It’s a big leap of faith, but that’s how we’ve made strides in cancer. The same commitment is crucial for Alzheimer’s as we unfold innovative therapies."
The research conducted at UK is essential, not just for developing therapies but also for fostering a culture of hope and proactive treatment in Alzheimer’s care. The groundwork laid in these studies illustrates how the combination of addressing the complexities of brain diseases can lead to better treatment modalities.
As researchers look toward the horizon, buoyed by the FDA approval of lecanemab and promising new treatments, there’s belief that a shift is underway in how both clinicians and patients perceive Alzheimer’s disease. The toxic mindset of "therapeutic nihilism" must be dismantled; it’s time to recognize that proactive measures can and should be taken.
"Society faces an aging population, and it’s imperative we unite to confront these challenges," said Dr. Jicha. "We must give individuals the option of aggressive treatments; waiting on the sidelines is no longer acceptable."
As the era of disease-modifying therapies begins, the compelling insights drawn from cancer research may well be the catalyst needed to transform the treatment landscape for Alzheimer’s disease. The path forward is fraught with challenges, but the dedication of researchers and the resilience of patients can usher in a new dawn of hope for combating this devastating disease.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)