Revolutionary Predictive Model Unveils COVID-19 Outcomes Based on Infection 'Signatures'
2024-10-31
Author: Rajesh
Revolutionary Predictive Model Unveils COVID-19 Outcomes Based on Infection 'Signatures'
In the tumultuous early days of the COVID-19 pandemic, one of the most critical challenges was forecasting patient outcomes: could doctors determine who would survive the infection and who would not? Four years later, while life-saving treatments and a robust vaccination effort have significantly mitigated fatalities, the science of predicting COVID outcomes is still evolving.
A groundbreaking study emerging from an international collaboration between researchers in Scotland and Brazil presents a novel predictive model that harnesses specific characteristics of SARS-CoV-2 infections. This model aims to forecast patient outcomes and improve triage processes in hospitals. The research, recently published in Science Translational Medicine, reveals insights derived from infections that occurred in 2020, raising important discussions about its applicability in our current vaccinated landscape as we approach 2024.
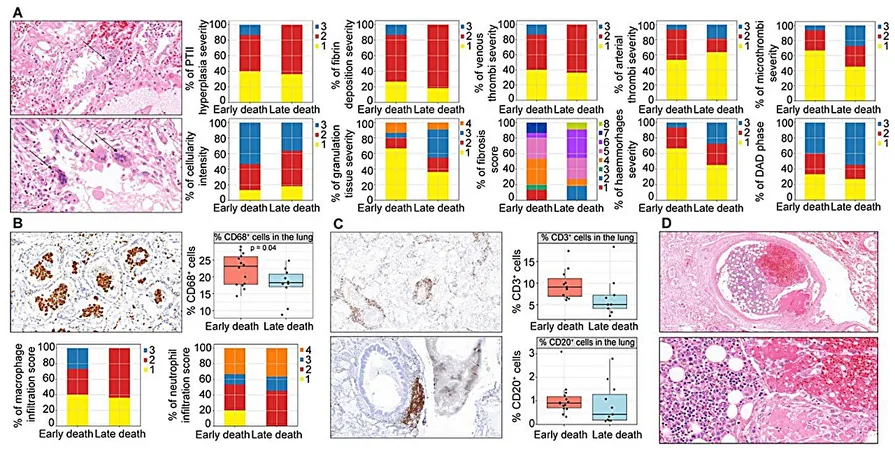
The modeling process hinges on identifying 'signatures' unique to COVID-19 infections. These biological markers were determined through the examination of data from 142 COVID patients in Brazil, where extensive clinical and blood data was analyzed both pre- and post-mortem. Findings indicate that certain biomarkers can predict a patient's trajectory upon hospital admission, categorizing them into groups like "early death," "late death," or "recovery."
Dr. João Da Silva Filho from the University of Glasgow has spearheaded this innovative research, stressing the importance of understanding how clinical biomarkers relate to lung pathology during acute phases of COVID-19. This understanding is pivotal for tailoring more effective treatments. His work, alongside collaborators from the University of Amazonas and the Federal University of Amazonas in Manaus, delineates the distinctive patterns of disease progression seen in patients.
"COVID-19 manifests through a wide array of symptoms and trajectories," Da Silva Filho asserts. "Our findings illuminate the critical interplay between clinical biomarkers and disease severity, paving the way for personalized medicine strategies."
The predictive model developed in this study highlights the stark differences between patients who recover from severe COVID and those who succumb to the illness. For instance, patients identified as "early death" exhibited dysfunctional immune responses marked by rapid endothelial activation and significant vascular inflammation leading to clot formation, while "late death" patients showed a different pathological landscape characterized by fibrosis and delayed immune responses.
Interestingly, the study also raises questions about the relevance of these findings in light of emerging COVID variants and the varying levels of immunity in the current population, largely due to widespread vaccination efforts and prior infections. Da Silva Filho and his team caution that their model is primarily based on patients treated during the first wave of the pandemic, and further research is needed to assess its predictive accuracy in today's context.
As we navigate a post-pandemic world, the insights garnered from this research not only have the potential to assist healthcare providers in triaging patients but also to inform the development of personalized treatment regimens. This advancement could serve as a game-changer in managing COVID-19 outcomes effectively, battling the virus with targeted precision based on the unique biological signatures of each patient.
For medical professionals and the general public alike, the implications of this research are profound. What remains to be seen is how swiftly the medical community can integrate such predictive tools into daily practice, enhancing patient outcomes and potentially saving lives in the continuing fight against COVID-19.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)