Revolutionary New Model to Identify Polycystic Ovary Syndrome Using France's National Health Database
2025-01-10
Author: Mei
Introduction
Polycystic ovary syndrome (PCOS) is a prevalent endocrine disorder that impacts countless women from adolescence through adulthood. While PCOS has been recognized for over three decades, the diagnostic criteria have evolved significantly.
Diagnostic Criteria of PCOS
Initially developed in 1990 by the National Institute of Health (NIH), the diagnosis relied on identifying both ovulatory dysfunction and signs of androgen excess. Major revisions occurred in 2003 when the European Society for Human Reproduction and Embryology (ESHRE) and the American Society for Reproductive Medicine (ASRM) introduced the Rotterdam criteria, underscoring the need for two of three characteristics: hyperandrogenism, ovulatory dysfunction, or polycystic ovarian morphology. In 2006, the Androgen Excess Society (AES) added that hyperandrogenism must be a defining condition.
Health Implications of PCOS
Before diagnosing PCOS, healthcare providers must exclude alternative causes such as thyroid disorders, hyperprolactinemia, and adrenal tumors. The implications of PCOS are profound, leading to risks for thromboembolic diseases, infertility, increased pregnancy complications, and mental health challenges, including anxiety and depression. Furthermore, women with PCOS face long-term health issues like non-alcoholic fatty liver disease, obesity, metabolic syndrome, type II diabetes, and cardiovascular diseases.
Economic Burden of PCOS
An alarming statistic revealed by Ding and colleagues estimates the economic burden of PCOS in the UK alone to be around £237 million, driven predominantly by type II diabetes and acne among affected women. In the United States, annual healthcare costs linked to PCOS-associated comorbidities soared to $8 billion USD in 2020. It's worth noting that these figures may underrepresent the actual costs, as they were calculated using conservative prevalence estimates.
Prevalence of PCOS
Globally, the prevalence of PCOS has shown significant variation based on diagnostic criteria. A recent meta-analysis reported a prevalence of 6.2% using NIH criteria while noting higher rates of 19.5% and 15% according to ESHRE/ASRM and AES, respectively. Alarmingly, data from health claim databases in the US identified just 1.6% of PCOS patients, prompting a call for improved algorithms to identify women with this condition.
PCOS-ECO Study
To address this gap, our research department initiated the PCOS-ECO study, aimed at utilizing the French national health data system (SNDS) to identify women with PCOS and assess the economic burden of this disorder within the population from 2013 to 2022.
Study Objectives
The objectives of this pivotal study included estimating the prevalence of PCOS in women aged 18 to 43 in France for the year 2021 via the ICD10 code E28.2, while also developing a robust case-finding algorithm and validating its effectiveness through a retrospective cohort study.
SNDS Database
The SNDS database encompasses a vast array of medical data for nearly the entire French population, offering a unique opportunity to perform in-depth analyses. Our preliminary results identified only 2,807 women (0.01%) with PCOS using the ICD-10 code, highlighting the pressing need for enhanced identification methods.
Algorithm Development
We meticulously crafted a comprehensive algorithm incorporating medical care consumption patterns associated with PCOS, utilizing relevant ICD-10 codes, treatment protocols, and laboratory tests. Our algorithm integrates criteria such as medical treatments for infertility, indications of hirsutism, and hormonal evaluations to refine detection.
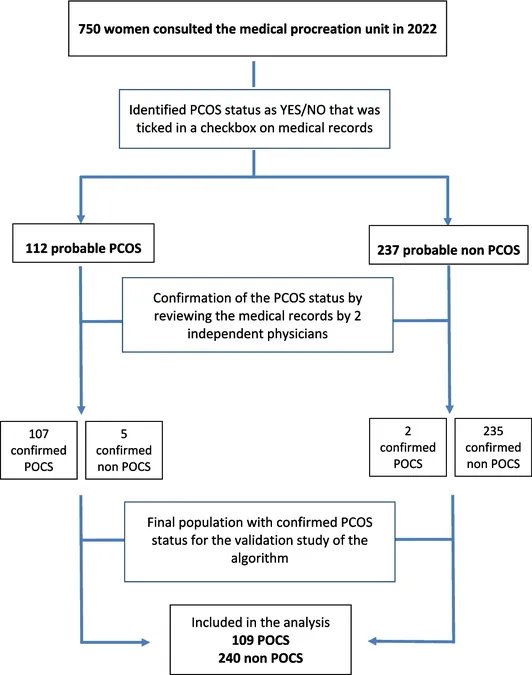
Internal Validation
Furthermore, our internal validation study focused on women who accessed assisted reproductive services, resulting in the identification of 109 true PCOS cases. Impressively, our algorithm demonstrated a sensitivity of 85% and a specificity of 96%, supporting its reliability in effectively identifying women likely suffering from PCOS.
Conclusion
The statistics reveal a complete necessity for a systematic approach to identifying PCOS within the healthcare system. As the burden of diseases associated with PCOS significantly impacts health outcomes and healthcare expenditures, tailoring better detection algorithms and interventions for this patient group is crucial.
Future Directions
The algorithm developed in this study holds promise beyond France; it could prove applicable across various healthcare systems worldwide. Future investigations should aim to validate this model on a broader scale as a means of alleviating the significant burden faced by women with PCOS.
Stay Tuned
Stay tuned for updates on how this groundbreaking study could change the lives of women worldwide!
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)