Revolutionary Follitropin Alfa Biosimilar Could Transform Fertility Treatments in France
2024-09-30
Introduction
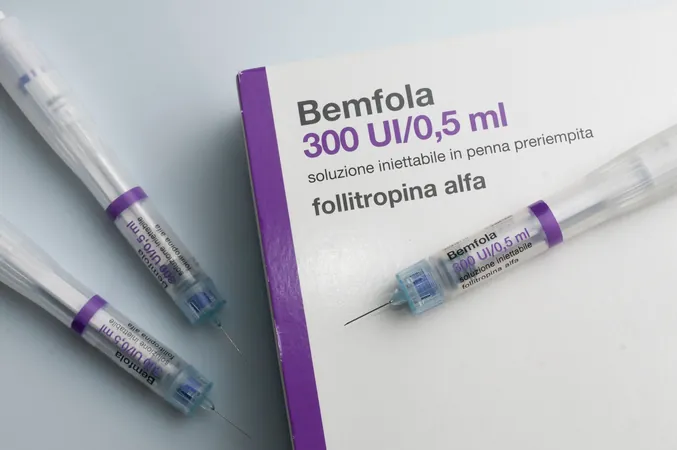
Recent research published in the *European Journal of Obstetrics & Gynecology and Reproductive Biology* has unveiled that the follitropin alfa biosimilar, known as Bemfola, is significantly more cost-effective than its original counterpart when it comes to ovarian stimulation. This analysis, viewed from the perspective of French healthcare payers, highlights that patients could save substantially while increasing the chances of successful pregnancies.
Infertility and ARTs
Globally, infertility remains a pressing issue, impacting approximately 1 in 6 individuals. Social stigmas often accompany this struggle, adding emotional strain to the high financial costs associated with assisted reproductive technologies (ARTs). The Centers for Disease Control and Prevention (CDC) defines ART as a combination of medical procedures, wherein eggs are retrieved from a woman’s ovaries, fertilized with sperm in a laboratory, and subsequently transferred back to the woman or donated, in hopes of achieving pregnancy.
Financial Burdens of ART
Despite their success rates, ART procedures can create financial burdens primarily due to the cost of follicle-stimulating hormones (FSHs). Recognizing this challenge, French health authorities have promoted the use of biosimilars as an economical alternative to alleviate these expenses. The introduction of Follitropin alfa biosimilar in 2015 marked a milestone, being the first recombinant human FSH available in France.
Study Overview
The focus of the recent study was a cost-effectiveness analysis comparing the follitropin alfa biosimilar with its originator for women undergoing in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI). The researchers created a decision-tree model evaluating total costs and cumulative live-birth rates (CLBRs) based on real-world data collected through France's REOLA study, which leveraged anonymous patient management systems.
Findings
The financial comparison revealed that the total costs per live birth amounted to €18,147 ($20,200) with the biosimilar, contrasted with €18,834 ($20,965) for the originator. This indicates a savings of €687 ($764) per live birth achieved through the use of the biosimilar—9.1% less expensive than its counterpart, primarily due to lower drug costs during the stimulation phase.
Potential Savings
Moreover, when accounting for potential drug wastage, savings could soar between €796 ($886) and €1,155 ($1,285) per live birth. If the follitropin alfa biosimilar were used universally in the REOLA study population of 6,606 women, the hypothetical savings would reach approximately €4,538,322 ($5,051,833), translating to an impressive increase of 250 live births. Extending this model across France could equate to a massive public health savings of €13,994,190 ($15,577,632), potentially resulting in 771 additional successful pregnancies.
Product Differences
Notably, the originator product is typically sold in multidose, multiuse pens, while the biosimilar allows physicians to customize pen sizes according to patients' specific needs, which can significantly reduce wastage.
Study Limitations and Conclusion
While the study presented promising findings, it acknowledged certain limitations, including reliance on assumptions that may introduce bias. Nonetheless, the results inspire hope for more cost-effective infertility treatment options within the French healthcare system. This groundbreaking research marks the first comprehensive economic analysis grounded in real-world data regarding CLBRs, providing a clearer picture of the sustainability and affordability of fertility treatments in France. As more healthcare systems consider biosimilars, patients may benefit from improved access to necessary reproductive treatments without the excessive financial burden typically associated with fertility interventions.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)