Revolutionary Findings in Alzheimer’s Disease: Microglial Response Unraveled!
2025-03-06
Author: Li
Transforming Immunotherapy for Alzheimer's
For many years, researchers have been striving to counteract the detrimental effects of Aβ accumulation, a hallmark characteristic of Alzheimer’s disease. Initially, active immunization techniques like AN1792, pioneered by Elan Pharmaceuticals, showed promise in reducing plaques but fell short due to severe inflammatory side effects. This setback led to the exploration of passive immunization treatments such as lecanemab, which zeroes in on Aβ protofibrils and aims to slow cognitive deterioration.
In the study led by Dr. David Gate, the research team examined brain tissue samples from patients who had undergone treatment with both therapies. By scrutinizing brain sections rich in Aβ plaques treated with lecanemab, the researchers analyzed over 14,000 spatial transcriptomics spots, revealing several unique microglial states associated with immune functionality in various cortical layers and white matter regions. Notably, these areas exhibited clusters of microglia expressing genes tied to crucial immune pathways—specifically complement signaling and lipid metabolism—essential for the clearance of Aβ.
When comparing the effects of AN1792 and lecanemab, the researchers discovered both overlapping and unique molecular markers activated by each treatment. While both approaches appeared to stimulate genes like APOE and TREM2—key players in recruiting microglia and clearing plaques—the research highlighted their differing approaches. AN1792 was linked with a greater expression of FAM107A, while lecanemab notably boosted SPP1 and LIPA, focusing more on lysosomal activity and lipid pathways.
Understanding the Immune Landscape in Alzheimer’s
Adding a vital layer of complexity, the study incorporated protein-level data, uncovering elevated levels of crucial immune proteins in plaque-laden regions—especially within the hippocampus and temporal cortex. Among these was HLA-DRA, pivotal in antigen processing, alongside CD68, a marker for phagocytic microglia. Interestingly, levels of the immune checkpoint protein PD-L1 decreased in areas of significant plaque clearance, indicating a carefully maintained balance between immune activation and inhibition.
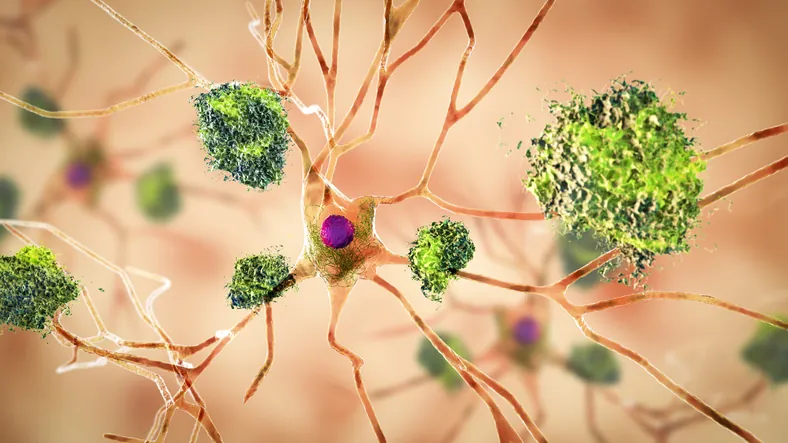
High-resolution imaging techniques corroborated these findings, demonstrating the clustering of microglia near plaques in lecanemab-treated brains, with notable expression of SPP1 and APOE. This supports the notion that microglia play a crucial role in both clearing plaques and facilitating tissue repair.
Paving the Way for Tailored Therapies
The research revealed essential insights about the delicate interplay between Aβ clearance and immune activation. In areas treated with lecanemab, extensive plaque clearance correlated with subdued inflammation and heightened repairs. Conversely, regions with poor clearance exhibited signs of elevated inflammatory pathways, underscoring the necessity to fine-tune treatments to minimize neurotoxic risks while enhancing effective plaque elimination.
By mapping the distinct gene expressions and adaptive states of microglia, this study lays an essential foundation for the development of precision-targeted therapies. Significant genes such as APOE, TREM2, SPP1, and FAM107A emerge as potential biomarkers that could help track treatment efficacy and tailor interventions to the unique needs of individual patients.
These findings illuminate the dual role of microglia as guardians against Aβ while also highlighting their involvement in inflammation. With ongoing refinements in immunotherapy strategies, a thorough understanding of this complex balance will be paramount to improving Alzheimer’s care. Harnessing the innate immune capabilities of the brain, this research represents a pivotal advance toward safer and more effective treatments, inspiring hope for millions facing this life-altering disease.
Stay tuned as the fight against Alzheimer’s disease pushes forward with relentless vigor!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)