Revolutionary Drug Combination Could Make Glioblastoma Cells Vulnerable to Immune Attacks
2024-11-08
Author: Jia
Introduction
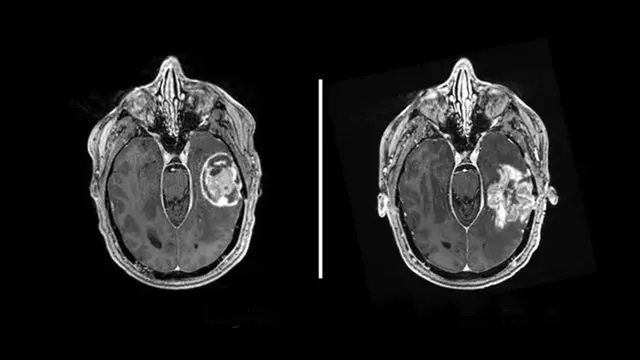
Glioblastoma, the most aggressive form of brain cancer, presents one of the most formidable challenges in oncology, with patients typically facing a grim prognosis of less than two years post-diagnosis, even with the most cutting-edge treatments. Traditional immunotherapies often falter in the face of glioblastoma due to the cancer cells lacking identifiable targets for immune system attack. However, groundbreaking research from Washington University School of Medicine in St. Louis reveals a promising strategy that could turn the tables on this relentless disease.
Study Overview
In a recent study published in *Nature Genetics*, scientists have successfully manipulated glioblastoma cells to display specific immune targets, essentially making them visible to the immune system and vulnerable to potential immunotherapies. This innovative approach employs a dual drug regimen, both of which have already received FDA approval for use in other forms of cancer.
Expert Insights
Dr. Ting Wang, one of the leading authors of the study, emphasized the groundbreaking nature of their findings: “For patients whose tumors do not naturally produce targets for immunotherapy, we have demonstrated a method to generate them. Essentially, we are creating targets where none existed.” This discovery could signal a new era of targeted and precise therapies for cancers that are notoriously hard to treat.
Mechanism of Action
Central to the researchers' strategy is the manipulation of transposable elements, segments of DNA that can change position within the genome. These elements have a dual nature in cancer: while they can contribute to tumor development, they also present vulnerabilities that can be harnessed for therapeutic purposes. The research team discovered that transposable elements can induce the production of unique proteins — known as tumor antigens or neoantigens — which are typically absent in healthy cells.
Challenges and Solutions
However, glioblastoma cells often produce very few of these immune targets naturally. To combat this limitation, Dr. Wang and his colleagues, including co-senior author Dr. Albert H. Kim, employed a combination of two epigenetic drugs: decitabine, typically prescribed for myelodysplastic syndromes, and panobinostat, used in the treatment of multiple myeloma. These drugs can alter the epigenome, the regulatory layer of gene expression, allowing tightly packed DNA in glioblastoma cells to unfurl and produce the necessary neoantigens.
Potential Side Effects
While this discovery holds immense promise, the researchers caution that healthy cells may also produce these neoantigens when subjected to the same treatment, potentially leading to unwanted side effects. Therefore, they are currently exploring ways to precisely target the epigenetic therapies solely to tumor cells.
Future Directions
Innovative approaches are also underway using CRISPR gene-editing technology to selectively induce expression of neoantigens in a variety of cancer types. If successful, this strategy could unify treatment pathways for numerous patients, enabling broad-spectrum immunotherapy options that specifically target shared neoantigens while sparing normal cells.
Conclusion
Dr. Kim, who also directs the Brain Tumor Center at Siteman Cancer Center, notes that although advancements in glioblastoma treatment have lagged behind those for other cancers like melanoma, they are optimistic about the future. "With ongoing advancements in immunotherapy and epigenetic therapies, we are on the verge of significant breakthroughs in how we treat glioblastoma," he stated. As research continues, the potential for this innovative drug combination to change the landscape of glioblastoma therapy remains an exciting possibility, offering hope to patients facing this daunting diagnosis. Stay tuned for updates as clinical trials may soon emerge from this groundbreaking research!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)