Revolutionary Discovery: New Sugar Molecule Could Change the Game for Pancreatic Cancer Treatment
2025-09-19
Author: Daniel
A Deadly Challenge: The Struggle Against Pancreatic Cancer
Pancreatic cancer has emerged as one of the most lethal forms of cancer, with a mortality rate that eclipses all others. Its often asymptomatic nature in the early stages makes early detection nearly impossible, allowing the disease to metastasize and leading to grim outcomes for most patients.
Breaking Ground: The HSAT Discovery
A groundbreaking study from the Salk Institute and the University of California San Diego has unveiled a unique sugar molecule known as HSAT (antithrombin-binding heparan sulfate). This molecule could serve as a revolutionary therapeutic target for decelerating tumor growth and metastasis in pancreatic ductal adenocarcinoma, the most prevalent type of pancreatic cancer.
Research highlights that HSAT is primarily found in pancreatic cells during the early stages of cancer, but diminishes as the disease advances. This reduction is linked to increased inflammation and a heightened risk of cancer spread. The researchers propose that boosting HSAT levels may slow the progression of pancreatic cancer, with patients exhibiting higher HSAT showing improved survival rates.
HSAT: A Potential Biomarker in Cancer Detection
Moreover, HSAT has been identified in the plasma of cancer patients, suggesting its potential role as a biomarker for diagnosing and monitoring pancreatic cancer. These tantalizing findings were detailed in the Journal of Clinical Investigation on September 16, 2025.
Co-senior author Dannielle Engle elaborates, "We’ve significantly expanded our understanding of pancreatic cancer biology here. HSAT is much more prevalent than we previously thought, especially in cancer, and is crucial for combating disease progression."
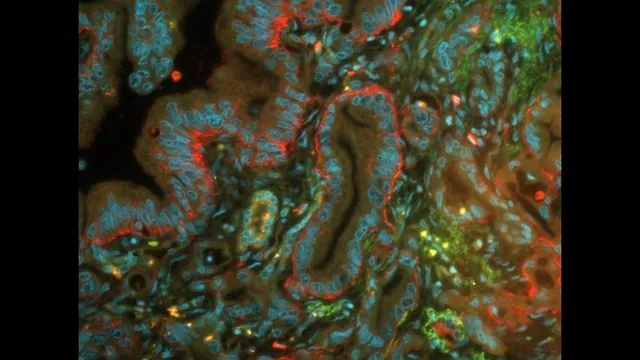
How Cancer Cells Transform: The Role of Surface Sugars
Cancer doesn’t just appear; it arises when normal cells mutate and start replicating uncontrollably, forming tumors. This transformation often involves changes to the cell's surface molecules, including sugars, which affect cellular behavior. In the case of pancreatic cancer, an overproduction of surface sugars allows cancer cells to evade the immune system, complicating treatment.
Blood Clots and Cancer: A Surprising Link
The study also draws intriguing connections between cardiovascular health and pancreatic cancer. Antithrombin, a protein crucial for blood clotting, interacts with HSAT. Enhancing HSAT levels may not only minimize the risk of clots in vulnerable cancer patients but could also slow cancer growth.
Thomas Mandel Clausen, another lead author, remarked, "Prior to our work, HSAT was considered rare in the body. We were surprised to find it abundant in various organs, particularly in pancreatic cancer cells, especially in early stages."
Unraveling HSAT’s Protective Role
The research analysis of human pancreatic tissues revealed a startling presence of HSAT not only in cancerous cells but also in healthy tissues. Significantly, patients with higher concentrations of HSAT had longer survival rates. The researchers further validated these findings using a mouse model.
Blocking HSAT led to increased tumor inflammation and a higher likelihood of metastasis, underscoring HSAT's crucial role in tumor suppression—a characteristic ripe for therapeutic manipulation.
The Future of Pancreatic Cancer Treatment
The study is a landmark achievement, proving that HSAT is not only widespread in epithelial cells but also crucial in preventing cancer progression. The possibility of using HSAT as a biomarker opens new avenues for diagnosing and monitoring pancreatic cancer at different stages.
As co-senior author Jeffrey Esko emphasizes, "If we can find ways to increase HSAT expression or screen for HSAT levels, we could potentially reduce pancreatic cancer mortality by improving early detection and treatment strategies."

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)