Revolutionary Deep Brain Stimulation Technique Transforms Walking for Parkinson's Patients
2025-07-22
Author: John Tan
Transforming Lives: A Breakthrough in Parkinson's Treatment
For individuals battling Parkinson's disease, the ability to walk can change dramatically. This condition, often characterized by a distinctive "Parkinson's gait," leads to altered step lengths and leg asymmetries, escalating the risk of falls and severely diminishing quality of life.
While high-frequency deep brain stimulation (DBS) has proven effective in alleviating tremors and stiffness, its benefits for gait issues have been inconsistent, especially in advanced cases. The absence of standardized metrics for gait assessment has posed considerable challenges in enhancing DBS outcomes for patients suffering from significant walking difficulties.
Innovative Machine Learning Approach
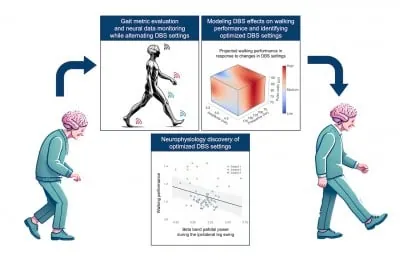
In an eye-opening new study from UCSF, researchers have pioneered a system to accurately quantify essential gait characteristics in Parkinson's patients. By harnessing machine learning, they identified tailored DBS settings that significantly improved walking conditions—resulting in faster, steadier steps without exacerbating other symptoms. The findings were published on June 18 in the prestigious journal, *npj Parkinson’s Disease*.
"We viewed optimizing DBS settings as an engineering challenge, seeking to model how stimulation parameters correlate with brain activity and walking performance," explains Dr. Hamid Fekri Azgomi, the study's lead author.
Insights into Gait Performance Optimization
The researchers implanted DBS devices that stimulate the brain and monitor neural activity during walking. By adjusting DBS settings at each clinical visit, they examined their effect on gait. Patients walked on a loop, with data captured continuously to assess their movement.
Using a newly developed Walking Performance Index (WPI), the study assessed various metrics including step length, stride velocity, and arm swing amplitude to provide a comprehensive view of gait dynamics disrupted by Parkinson's.
"Our results confirmed that the WPI effectively captured the impact of DBS adjustments, aligning with both patient and clinician feedback during visits," Azgomi says.
Uncovering Neural Patterns for Better Walking
Additionally, the team identified brain activity patterns associated with improved walking. Employing advanced models, they distinguished the neural dynamics that facilitate optimal walking performance, noting reduced beta-band brainwave activity linked to enhanced gait in the globus pallidus—a brain region critical for movement control.
These findings not only enhance our understanding of DBS’s effects but also emphasize the power of personalized, data-driven approaches to improving gait in Parkinson's patients.
A Promising Future for Personalized Treatment
Dr. Doris Wang, the senior author, states, "This research underscores the potential of personalized neuromodulation for Parkinson's and other neurological disorders, pushing us closer to more effective treatment methods."
Future research directions include creating real-time gait analysis systems and integrating the WPI with DBS programming tools. This could involve technologies like gait mats and wearable sensors for continuous, precise monitoring, leading to highly accurate DBS adjustments.
A New Dawn for Parkinson's Patients
These groundbreaking findings point to a bright future for transforming the walking abilities of Parkinson's patients, offering hope for improved mobility and quality of life.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)