Revolutionary Breakthrough: Scientists Create First Vascularized Organoid Model of Pancreatic Islets!
2025-05-23
Author: Li
A Groundbreaking Achievement in Diabetes Research!
In a monumental advancement, a team of international researchers led by Professor Maike Sander, MD, from the Max Delbrück Center, has successfully developed the world’s first organoid model of human pluripotent stem cell-derived pancreatic islets that features integrated blood vessels. This innovative model promises to transform our understanding of diabetes and pave the way for advanced therapies!
Mimicking Nature: The Key to Success!
Research from Sander's lab at the University of California, San Diego, reveals that these vascularized organoids not only contain a higher quantity of mature beta cells, which are essential for insulin production, but also exhibit superior insulin secretion compared to non-vascularized alternatives. The vascularization allows these organoids to more accurately replicate the functionality of actual pancreatic islet cells in the body.
A Giant Leap for Diabetes Research!
"Our findings underscore the critical role of a blood vessel network in enhancing the function of pancreatic islet cells," remarked Sander. "This model brings us significantly closer to creating conditions akin to those in the pancreas, vital for new diabetes treatments and research advancements." The team’s work, published in the journal *Developmental Cell*, indicates that these vascularized organoids can vastly improve our understanding of the interplay between beta cells and endothelial cells (ECs), offering a powerful platform for studying diseases and testing therapies.
Unlocking Potential: How They Did It!
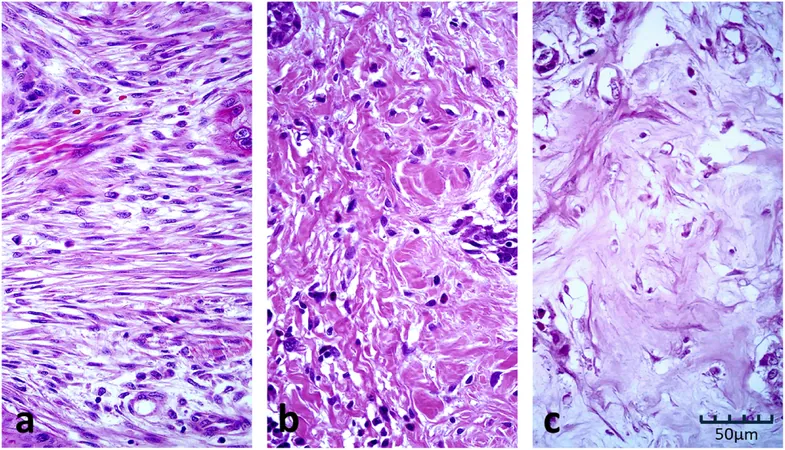
Pancreatic islets, clusters of hormone-producing cells, play a crucial role in regulating insulin levels in the body. However, existing organoid models typically suffer from immaturity of beta cells, limiting their effectiveness for real-world applications. The researchers ingeniously incorporated human ECs and fibroblasts into their stem cell-derived islet organoids, experimenting for five years with different environmental conditions until they discovered a specific cell culture medium that boosted both survival and maturation. This led to the creation of a sophisticated network of vascular structures penetrating the organoids.
A Breakthrough in Functionality!
The groundbreaking vascularized organoids not only matured more effectively but also demonstrated a striking increase in insulin secretion when exposed to elevated glucose levels. This contrasted sharply with their non-vascularized counterparts, indicating that the enhanced vascular structure fosters more mature beta cell functionality.
Revolutionizing Diabetes Models!
Researcher Sander emphasized the exciting revelations about how vascularization advances beta cell maturation. Key mechanisms include the stimulation of extracellular matrix formation and the secretion of bone morphogenetic protein (BMP) by endothelial cells, both critical to cell growth and development. Further, the team utilized microfluidic devices to simulate nutrient flow through the organoids, leading to an even higher proportion of mature beta cells.
Impacts on Diabetic Treatments!
In an impressive demonstration of the model’s viability, diabetic mice benefited significantly from grafted vascularized islets, with some showing no signs of the disease after 19 weeks. Sander’s insights into how crucial EC presence boosts beta cell functionality solidify belief in pre-vascularization as a game-changer for islet transplantation.
Future Endeavors: Aiming to Combat Type 1 Diabetes!
Harnessing this innovative model, Sander plans to delve into type 1 diabetes, where immune responses lead to beta cell destruction. By growing these vascularized organoids from the cells of type 1 diabetes patients and integrating them with patient-derived immune cells, the researchers hope to elucidate the mechanisms of beta cell attack.
A Vision for the Future!
Ultimately, Sander and her team aspire to refine this vascularized SC-islet organoid model to explore the complexities of pancreatic islet function and autoimmune beta cell destruction. This pioneering research redefines the landscape of diabetes models and holds immense promise for developing more effective treatments.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)