Revolutionary Biomarker Algorithm for Early Detection of Barrett's Esophagus and Esophageal Cancer Unveiled!
2025-01-22
Author: Li
In a groundbreaking development, researchers at the Johns Hopkins Kimmel Cancer Center and the Johns Hopkins University School of Medicine have created an innovative biomarker algorithm that holds the promise of transforming the early detection of esophageal cancer and precursor conditions like Barrett's esophagus (BE). This new method utilizes noninvasive techniques to collect esophageal cells, offering a potentially life-saving alternative to the traditional invasive endoscopy procedures that require patients to be anesthetized.
The findings, published on January 17 in the American Journal of Gastroenterology, suggest that this new algorithm could serve as an initial screening tool to determine which patients may require further evaluation by endoscopy. This could significantly reshape patient management and improve early detection rates in a field where time is of the essence.
Senior study author Stephen Meltzer, M.D., renowned for his work in gastrointestinal cancers, emphasized the rigorous approach taken to identify the biomarkers. He noted, "Our study represents the first comprehensive effort to select biomarkers specifically for Barrett's esophagus, esophageal adenocarcinoma, and high-grade dysplasia."
The algorithm identified critical biomarkers tied to methylation processes — a chemical change that influences gene expression and has been implicated in various cancers, including prostate, liver, and colorectal cancers. The team focused on three specific genes: USP44, TBC1D30, and NELL1, which have already been established as significant markers in cancer research.
Using data from the Gene Expression Omnibus database, the research team honed in on biomarkers that showed significant methylation differences between BE tissues and healthy controls. From an initial pool of 30 candidates, 12 were selected for further validation. Laboratory tests confirmed their elevated potency in identifying BE over normal esophageal tissues.
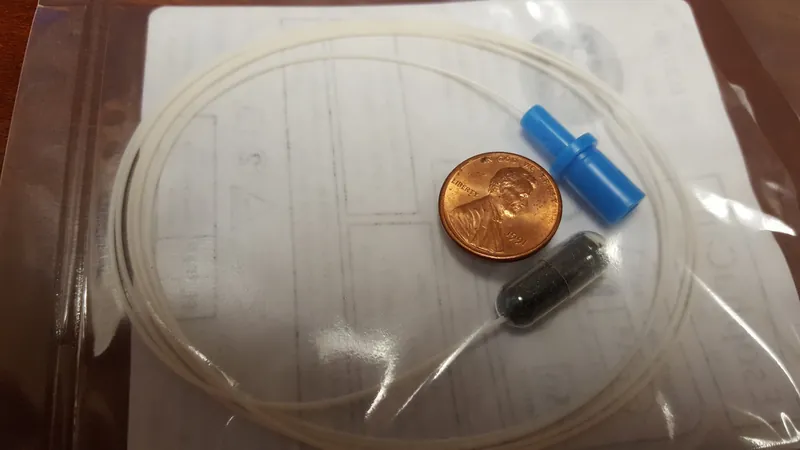
The research then utilized samples from 234 nonendoscopic esophageal sponge tests. Amazingly, patients voluntarily swallowed a small sponge contained within a gelatin capsule, which collected cells during its retrieval from the esophagus. This noninvasive method significantly reduces discomfort and risk compared to traditional endoscopies, while still providing crucial diagnostic information.
The study's participants, predominantly male and with a median age of 65, came from diverse backgrounds. After rigorous analysis, the findings resulted in a new three-biomarker algorithm, which performed stunningly well, achieving an area under the curve (AUC) score of nearly 0.97 for distinguishing healthy tissue from cancerous tissue.
Meltzer is optimistic about the potential of this sponge-biomarker test, stating, "This is not intended as a definitive diagnosis, but rather a signal indicating that a patient may require an endoscopy after abnormal findings."
With esophageal cancer cases surging fivefold in Western populations over the last 40 years, this advancement is timely. Currently the eighth most common cancer worldwide, early detection methods are crucial since approximately 5%-12% of individuals with gastroesophageal reflux disease (GERD) may develop Barrett's esophagus, a condition that often goes undiagnosed.
As researchers continue to validate their algorithm, the hope is to empower clinicians with better screening tools, potentially saving thousands of lives by catching esophageal diseases at their earliest, most treatable stages. Stay tuned as this promising technology unfolds!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)