Revelations on Bloodstream Infections in Pediatric Burn Victims in South Africa: A Call for Enhanced Antimicrobial Stewardship
2025-03-14
Author: Arjun
Introduction
Bloodstream infections (BSIs) are alarmingly prevalent among pediatric burn patients in low- and middle-income countries, significantly contributing to morbidity and mortality rates. This is particularly concerning as these infections frequently involve multidrug-resistant (MDR) pathogens such as Staphylococcus aureus, Escherichia coli, and Pseudomonas aeruginosa. With increasing cases of MDR BSIs, it is imperative to refine antimicrobial stewardship practices, potentially through more tailored initial antimicrobial therapies.
This article dives into the pathogens, timing, and implications related to burn-associated BSIs in children treated in two pediatric surgical units in Tshwane District, South Africa.
Methods
Our multi-centre retrospective review focused on pediatric burn patients aged 0-12 years admitted from January 2020 to December 2022. The study drew data from patient medical records and the National Health Laboratory System TrakCare database, adhering to CDC definitions for bloodstream infections.
Results
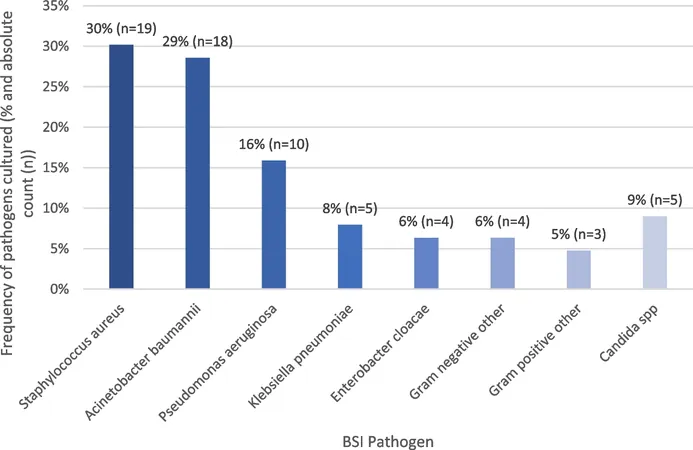
Out of 245 admitted pediatric burn patients, 18.8% (46 children) developed bloodstream infections. Among 63 positive blood cultures, the predominant pathogens identified included S. aureus (30%), Acinetobacter baumannii (29%), and P. aeruginosa (16%). Gram-negative bacteria were responsible for 65% of the infections. Notably, 56% of the pathogens were multidrug-resistant, including a significant number of methicillin-resistant S. aureus (MRSA) and carbapenem-resistant strains of A. baumannii. The analysis showed that gram-positive bacteria were leading causes early in the admission, while gram-negative and fungal infections emerged later.
Conclusion
Our findings indicate that both gram-positive and gram-negative infections predominantly manifest soon after burn injuries, suggesting that initial targeted antibiotic therapies may often be ineffective. Therefore, it is recommended that healthcare providers shift towards antimicrobial de-escalation strategies once culture results are available. Furthermore, proactive measures in wound care and infection control are essential in reducing the high incidence of BSIs, alongside responsible usage of broad-spectrum antibiotics to mitigate the rise of antimicrobial resistance.
The findings align with alarming statistics regarding pediatric burn injuries in low- and middle-income countries, where children under 10 represent the majority of cases and fatalities. Burn patients are particularly susceptible to infections due to compromised skin barriers and other risk factors such as young age, extensive burn surface area, and invasive medical devices.
Further Insights
The research highlights that early identification of bloodstream infections in burn patients is challenging, primarily due to the hyper-inflammatory response post-burn injury. Despite adherence to clinical guidelines for diagnosing BSIs, there remains a gap in timely identification and treatment, emphasizing the need for continuous monitoring and strict infection control protocols.
Additionally, this study uncovers the concerning trend of increasing antibiotic resistance among key pathogens impacting pediatric burn patients. The resistance rates observed necessitate a re-evaluation of current antimicrobial protocols and a stronger commitment to infection prevention initiatives within healthcare settings.
With the striking incidence rate of BSIs in pediatric burn cases, empowering healthcare workers with advanced training in infection control practices could vastly improve patient outcomes. This multifaceted approach could help combat the rising threat of MDR infections and ultimately save lives in vulnerable populations.
As we move forward, the healthcare community must prioritize research and implementation of effective antimicrobial stewardship programs tailored to the needs of burn care in developing regions. This critical shift could hold the key to overcoming one of the most pressing challenges faced by pediatric burn patients and healthcare systems alike.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)