Revealing the Truth: Are Countries Really Prepared for the Next Pandemic?
2024-11-07
Author: Siti
Introduction
In an era where infectious disease outbreaks threaten global health, the spotlight is shining brighter than ever on nations' preparedness and response capabilities. Recent analysis covering 186 countries between 2018 and 2022 has unveiled staggering statistics that everybody needs to know—over 6.9 million deaths worldwide have been attributed to the COVID-19 pandemic, making it essential for countries to strengthen their health systems in anticipation of future public health emergencies.
Emerging Infectious Diseases
Emerging infectious diseases are on the rise, propelled by various factors such as increased global travel, trade, and encroachment into wildlife habitats due to urbanization and agricultural expansion. This disturbing trend is likely to worsen as climate change continues to disrupt ecosystems, fostering viral spillover events where diseases jump from animals to humans. As conditions become more conducive for diseases like dengue, Zika, and Lyme disease, the peril of infectious outbreaks looms larger than ever.
International Health Regulations and Global Preparedness
The International Health Regulations (IHR) of 2005 require countries to maintain certain core capabilities to adequately address public health risks. Yet, a shocking proportion of global populations reside in nations lacking robust surveillance and response systems. Countries are required to self-report their health security capacities through a tool known as the State Party Self-Assessment Annual Reporting (SPAR). However, discrepancies abound in the accuracy of these self-reports, with some nations inflating their capabilities.
Investment vs. Capability
Despite significant investment in capacity-building initiatives, a troubling number of countries remain ill-equipped to manage infectious disease threats. Many nations are still struggling with fundamental public health surveillance, as illustrated by the challenges faced during the 2009 H1N1 pandemic and the 2014-2015 West Africa Ebola outbreak. The necessity for continuous monitoring and improvement in IHR response capacities can’t be understated; the society’s reliance on timely and effective health interventions is imperative, especially given that outbreaks can occur unexpectedly.
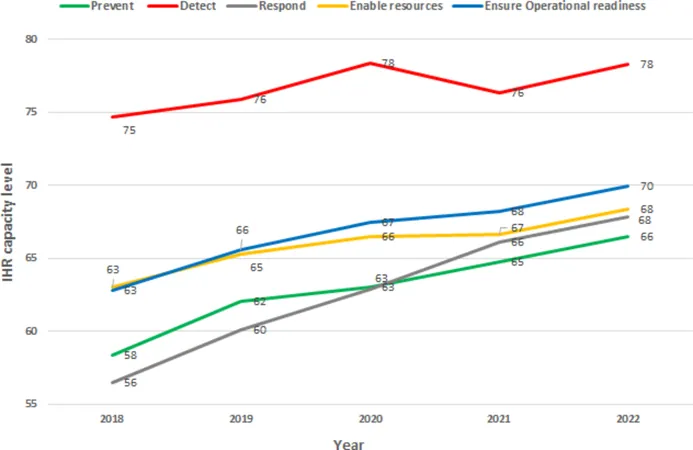
Analysis of SPAR Submissions
Through meticulous analysis of SPAR submissions from 2018 to 2022, researchers have formulated critiques highlighting both gains and grievous gaps in global health security. There was a noteworthy improvement in preventive capabilities, evidenced by a rise in the global health security capacity score from 58.4 in 2018 to 66.5 in 2022. However, when it came to the ability to detect public health risks, the results were disappointing, with no statistically significant improvement over the study period.
Regional Disparities in Preparedness
The report identified regions with the highest and lowest preparedness levels. High-income countries like Canada, Denmark, and Russia topped the charts, while low-income nations in sub-Saharan Africa consistently demonstrated inadequate capabilities. Alarmingly, in 2022, only 34% of countries in the African region maintained functional capacity to prevent public health events. Comparatively, advanced economies showed significantly better preparedness, highlighting dire inequalities.
Vulnerability of African Nations
This alarming disparity raises critical questions regarding the regions most vulnerable to health crises. Countries in Africa, facing challenges like high rates of malnutrition and endemic diseases, are vying for resources like medical supplies and skilled personnel with wealthier nations. The relative immunity to COVID-19 seen in some African nations may have unwittingly slowed their progress in enhancing health security capabilities, calling for urgent action to rectify systemic weakness and vulnerability.
The Need for Change
Looking ahead, the findings emphasize an urgent need for an overhaul of pandemic preparedness measures. The call to action is clear: Wealthy nations must bolster their support to developing countries to enhance their public health systems. Investments in digital health technologies and comprehensive disaster risk reduction strategies hold tremendous promise for creating resilient health systems that are capable of enduring future public health threats.
Conclusion
The road to achieving global health security is fraught with challenges, but with dedicated effort and international cooperation, it is within reach. As the world braces for the next inevitable epidemic, the question remains: Are we ready to confront it? Don’t be caught off guard—stay informed and advocate for stronger global health policies!





 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)