Psychological Stress: The Hidden Trigger Behind Food-Induced Symptoms in IBS
2025-03-17
Author: Mei
Psychological Stress: The Hidden Trigger Behind Food-Induced Symptoms in IBS
In a groundbreaking study recently published in Gastroenterology, scientists have uncovered compelling evidence that psychological stress can activate immune responses to food, leading to distressing symptoms when that food is consumed again. These findings shine a light on the significant role stress plays in irritable bowel syndrome (IBS), a condition that continues to baffle researchers and patients alike.
Dr. Cecilia Berin, a leading researcher and co-author of the study, emphasized the broader implications of these findings. "This study highlights the key role that activation of the immune system by food plays in many diseases beyond those that we typically think of as food allergies," she explained. "It’s revealing a molecular explanation for why food can trigger not only allergies but also pain experienced in IBS."
Previous research indicated that bacterial infections could result in the development of immune responses and allergic reactions to food antigens, which manifest as abdominal pain, a hallmark symptom of IBS. Furthermore, while it's established that IBS may develop following infections, this accounts for only a fraction of IBS cases, leaving many patients grappling with unexplained symptoms.
To delve deeper, the researchers set out to explore whether analogous immune responses triggered by psychological stress could worsen food-induced pain. Dr. Berin elaborated, "Psychological stress can directly impact the physiology of the gastrointestinal tract."
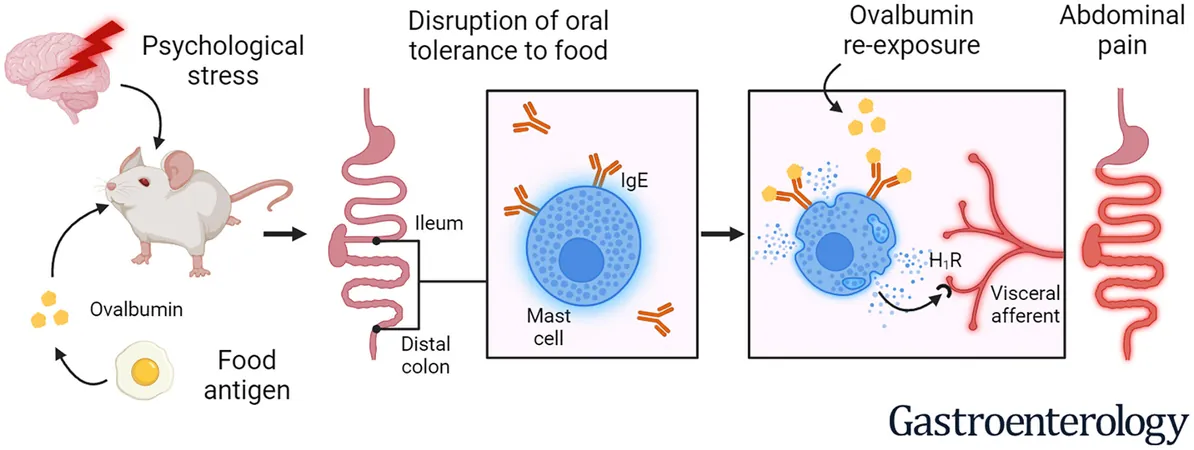
In their experimental setup, researchers exposed mice to ovalbumin – a protein found in egg whites – during a stress-inducing test known as water avoidance stress. After a period of five weeks, these mice were re-exposed to ovalbumin.
The team then rigorously measured visceromotor responses (abdominal contractions) and nerve activity in response to intestinal distension. They aimed to understand how these processes relate to nociception – the nervous system's response to potentially harmful stimuli. Their findings indicated that the earlier exposure to ovalbumin, coupled with stress, significantly increased pain signaling in the mice's colon and small intestine.
Moreover, the study revealed that this pain response was intricately linked to mast cells (a type of white blood cell), local IgE antibodies, and signaling pathways involved in immune responses. Notably, the application of pyrilamine, an existing medication for allergy symptoms, was found to inhibit heightened sensory neuron activity and alleviate nerve firing in response to intestinal distension.
Dr. Berin noted the surprising nature of these results, highlighting that allergic reactions could alter normal gastrointestinal function and lead to pain without eliciting systemic allergic reactions, like anaphylaxis. "The fact that IgE antibodies, which typically trigger allergic reactions, were at the heart of these symptoms in a context distinct from food allergies is intriguing," she remarked.
As the research progresses, the next steps will involve examining gastrointestinal immune cells from patients with IBS. This could offer crucial insights into whether localized food-specific immune responses are similarly present in human cases.
Overall, this study opens the door to new understandings of IBS and its triggers, potentially paving the way for innovative treatments targeting the intersection of psychological stress and gastrointestinal health. Future research could be pivotal in helping millions who suffer from this often invisible and debilitating condition.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)