Patients with Myelodysplastic Syndromes Report Higher Symptom Frequencies Than Physicians Recognize
2024-11-02
Author: Wei Ling
Introduction
A new report reveals a troubling disparity between patients with myelodysplastic syndromes (MDS) and their physicians regarding the frequency and severity of symptoms. Published in the journal *Oncology and Therapy*, the study is rooted in questionnaires completed by both patients and physicians across the United States and Europe.
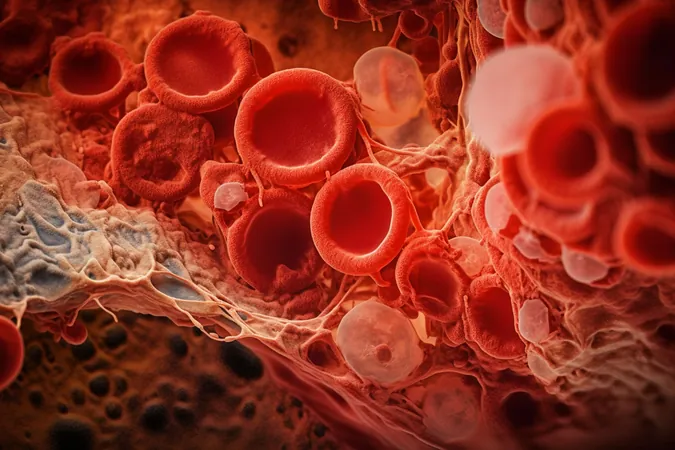
Understanding Myelodysplastic Syndromes (MDS)
Myelodysplastic syndromes represent a group of bone marrow disorders that primarily affect the blood's ability to produce healthy cells, leading to symptoms like fatigue, weakness, and increased bruising. The only potential cure for MDS is allogeneic hematopoietic stem cell transplantation, which is often reserved for younger patients or older, healthier individuals at risk of developing acute myeloid leukemia (AML). Alarmingly, the median age for MDS diagnosis is 70, which means a significant number of individuals may be considered too old or unfit for this procedure.
Treatment Approaches
For patients categorized as low-risk, the focus of treatment is typically on enhancing quality of life rather than curative measures. Conversely, patients with high-risk MDS are often treated with hypomethylating agents aimed at extending survival and managing disease progression—the five-year survival rate for MDS remains a dismal 30%.
Impact on Quality of Life
The report highlights that many patients endure a dramatically decreased quality of life, with fatigue and shortness of breath being particularly debilitating. Psychological challenges, including anxiety and depression, are also common among this demographic. The authors sought to investigate not only the burdens of MDS on patients but also the alignment between patients' and physicians' perceptions regarding these burdens.
Research Methodology
To do this, researchers collected health data from US and European physicians for 1,445 MDS patients, who were then invited to complete detailed questionnaires, alongside their caregivers. The findings revealed that over half of the patients (52%) were on supportive treatments, with high-risk patients significantly more likely to receive anti-AML therapies and transfusions than their low-risk counterparts.
Discrepancy in Symptom Recognition
An interesting aspect of the study was the discordance between patient-reported symptoms and the physicians’ understanding. Patients were more likely to report issues like excessive bruising and gastrointestinal problems, highlighting a crucial gap in communication that demands attention. Among high-risk MDS patients, this discrepancy was notably pronounced, suggesting a necessary push for better dialogue between patients and their healthcare providers.
Caregiver Burden
Caregiver burden also emerged as a significant factor, with caregivers spending an average of 42 hours per week for low-risk patients and 49.3 hours for high-risk patients. Physicians, however, greatly underestimated this need, indicating a significant knowledge gap on caregiver workload—particularly concerning younger caregivers, who often juggle work commitments with caregiving duties.
Conclusion
The authors concluded that the healthcare community must enhance communication, offering patients and their families clearer insights into treatment options and expected outcomes. Additionally, they urged for advancements in MDS therapies to improve patients' experiences and quality of life. As the healthcare landscape continues to evolve, understanding and addressing the needs and challenges faced by both patients and caregivers become paramount, shedding light on the need for empathetic and informed medical care.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)