New Study Reveals How the APOE4 Gene Fuels Alzheimer's Damage through Brain Immune Cells
2024-11-04
Author: Mei
Introduction
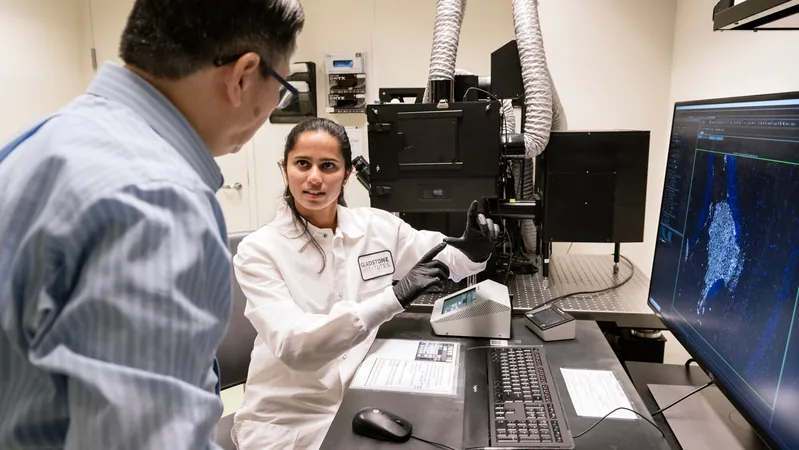
Recent research from the Gladstone Institutes shines a light on the double-edged sword of brain immune cells in the context of Alzheimer's disease, particularly focusing on the APOE4 gene—the most significant genetic risk factor for this devastating illness.
Role of Microglia in Healthy Brains
In healthy brains, microglia, a type of immune cell, act as vigilant guardians, clearing out debris and harmful proteins. However, the presence of the APOE4 protein takes a dark turn; the same microglia become agents of inflammation and contribute to the formation of toxic protein clumps, as revealed by a groundbreaking study.
Innovative Research Model: The Chimeric Mouse
To explore the intricate relationship between APOE4 and brain cells, researchers devised an innovative research model. They transplanted human neurons that produce the APOE4 protein into the brains of mice. The results were illuminating: when microglia were removed, the abundance of amyloid and tau deposits—two hallmark proteins of Alzheimer's—was significantly reduced. “This study underscores the pivotal role of both microglia and APOE4-producing human neurons in driving Alzheimer's pathology,” stated Dr. Yadong Huang, the senior investigator behind the study published in *Cell Stem Cell*.
Understanding APOE Variants
Humans possess three major forms of the APOE protein: APOE2, APOE3, and APOE4. While APOE3 is the most common variant, APOE4 dramatically heightens the risk of Alzheimer’s. About 25% of Americans carry at least one copy of the APOE4 gene, with those possessing two copies facing a staggering 12-fold increase in their risk of developing the disease.
Unveiling the Mechanism of Damage
The research team has long relied on mouse models, yet replicating human neurological conditions in mice has proven challenging. Traditional methods often fell short, as merely introducing the APOE4 gene into the mice didn't adequately reflect how human brain cells functioned in Alzheimer’s. The newly developed 'chimeric' model incorporates human neurons, providing a closer approximation of the late-onset Alzheimer’s experienced by older adults.
Key Findings
Experiments confirmed that mice with human APOE4 neurons exhibited heightened levels of amyloid plaques and tau tangles as they aged, revealing the direct correlation between APOE4 and Alzheimer’s characteristic protein accumulations.
The Dark Side of Microglia
The team discovered that human neurons producing APOE4 activate microglia, leading these immune cells down a harmful path. Utilizing advanced tools such as single-cell RNA sequencing, they identified that the presence of APOE4 resulted in an inflammatory environment, whereby up to 30% of microglia in those with human APOE4 neurons displayed the most inflammatory molecular signatures.
Implications for Alzheimer's Pathology
This transformation highlights a crucial aspect of Alzheimer's pathology: microglia, typically protectors of the brain, can become harmful when stimulated by the APOE4 protein.
Hope for Future Treatments
Excitingly, these findings open avenues for potential treatments targeting this vicious cycle. By curbing the inflammatory response of microglia or reducing the levels of APOE4 within neurons, researchers might be able to slow down or prevent the progression of Alzheimer’s in genetically at-risk individuals.
Next Steps
While these strategies are promising, further research is needed to evaluate their effectiveness in humans, the potential side effects, and optimal timing for intervention. The team's next steps will involve leveraging this sophisticated chimeric mouse model to investigate other cell types' roles within the complex Alzheimer's disease landscape.
Conclusion
In conclusion, this innovative research not only enhances our understanding of the link between the APOE4 gene and Alzheimer’s disease but also paves the way for developing targeted therapies that could revolutionize the treatment of this incurable condition. Keep an eye on these developments; they might just change the game in Alzheimer’s research!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)