New Study Links C-Reactive Protein-Triglyceride Glucose Index to Increased Stroke Risk in Different Glycemic Stages!
2025-03-26
Author: Sarah
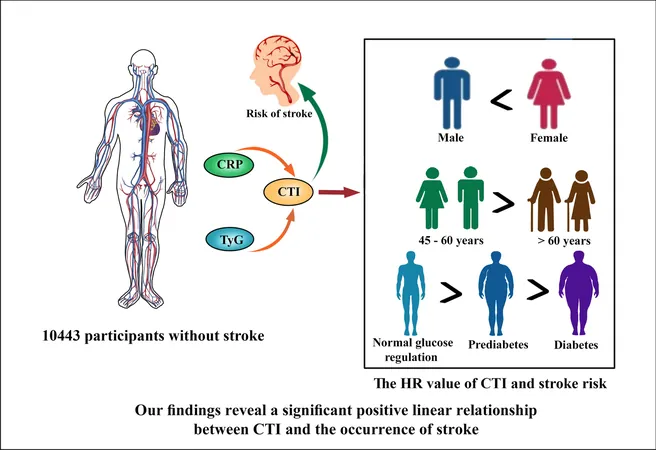
A groundbreaking new study published in the esteemed China Health and Retirement Longitudinal Study (CHARLS) explores the alarming association between the C-reactive protein-triglyceride glucose index (CTI) and the risk of stroke across various glycemic statuses. This significant research reveals that even mild elevations in CTI could spell disaster for some populations, raising a vital red flag for healthcare professionals regarding stroke prevention.
What is Hypertension and Diabetes?
The study defines hypertension as occurring in individuals with a systolic blood pressure (SBP) greater than or equal to 140 mmHg, diastolic blood pressure (DBP) of 90 mmHg or higher, self-reported hypertension from a physician's diagnosis, or those currently on antihypertensive medication. On the other hand, diabetes mellitus (DM) was identified by fasting plasma glucose levels equal to or higher than 126 mg/dL, an HbA1c of at least 6.5%, or the use of antidiabetic medications. Pre-diabetes (Pre-DM) was characterized by glucose levels falling between 100 and 125 mg/dL.
Key Study Findings
The research analyzed data from 10,443 Chinese adults, whose average age was 59 years, with nearly half of the participants being male. The findings were startling: during a follow-up period of approximately nine years, 960 individuals experienced their first stroke. The incidence of stroke increased across the CTI quartiles, with a staggering 12.3% occurring in the highest quartile compared to just 6.0% in the lowest.
1. **Significance of CTI**: Each one-unit increment in CTI correlated to a **19% higher risk of stroke** (HR 1.19). This risk rose even more dramatically in individuals with higher CTI levels—showing a clear pattern of increased risk with greater CTI scores.
2. **Impact on Different Demographics**: The link between CTI and stroke risk was consistent across genders, though women showed a slightly higher hazard ratio (HR 1.22) compared to men (HR 1.15). Similarly, middle-aged individuals (45-60 years) had a higher risk compared to those over 60 (HR 1.25 vs. HR 1.12).
3. **Glycemic Status Matters**: Intriguingly, the study found that individuals with normal glucose regulation (NGR) and Pre-DM experienced significant stroke risk increases with rising CTI levels. Specifically, a one-unit increase in CTI was associated with a 33% increased stroke risk in NGR individuals and a 20% increase for those with Pre-DM. However, no such association was found in participants with diabetes.
Understanding the Mechanism
Although the detailed mechanisms remain unclear, the study suggests that insulin resistance and inflammation might contribute to endothelial dysfunction and atherosclerosis, increasing stroke risk. Furthermore, the combined CTI index, which incorporates both inflammation and insulin resistance markers, paints a more comprehensive picture of cardiovascular health compared to conventional measures.
Implications for Healthcare
Given the study's robust findings—alongside a strong background in existing literature linking TyG index and stroke risk—this research underscores the urgent need for healthcare providers to focus on monitoring CTI levels, especially among middle-aged and younger women. Additionally, proactive measures should be considered for managing CTI levels among individuals with NGR and Pre-DM to mitigate stroke risks effectively.
The Road Ahead
This comprehensive analysis not only sheds light on the CTI's predictive power for stroke risk but also advocates for meticulous patient management regarding lifestyle intervention strategies aimed at reducing inflammation and enhancing metabolic health. Future research should focus on investigating the mechanisms behind the CTI and its role across diverse populations and clinical settings—ultimately leading to improved outcomes for at-risk patients.
Stay tuned for more exciting findings in health research! This significant study opens doors to new preventative strategies and forms a critical part of the ongoing conversation about stroke risk management in clinical practice.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)