New Insights on the Effectiveness of PHQ-9 and GAD-7 in Detecting Depression and Anxiety in Chinese Youth
2025-03-29
Author: Mei
Depression and anxiety pose significant mental health challenges, ranking among the leading causes of illness and disability for young people globally. A meta-analysis highlights global prevalence rates of 2.6% for depression and 6.5% for anxiety among children and adolescents. In China, these numbers registered slightly higher—3.0% and 4.7%, respectively. Early onset of these disorders threatens academic performance, interpersonal relationships, substance abuse, and often carries consequences that extend into adulthood, including a concerning increase in suicidal ideations.
Effective screening for depression and anxiety is crucial for early diagnosis and treatment. Among the various tools available, the Patient Health Questionnaire-9 (PHQ-9) for depression and the Generalized Anxiety Disorder-7 (GAD-7) for anxiety are highly regarded for their brevity and reliability, initially designed for adult patients. While adaptations for children and adolescents have been validated, emerging studies reveal alarming discrepancies in their effectiveness when used within this age group, particularly in Chinese populations.
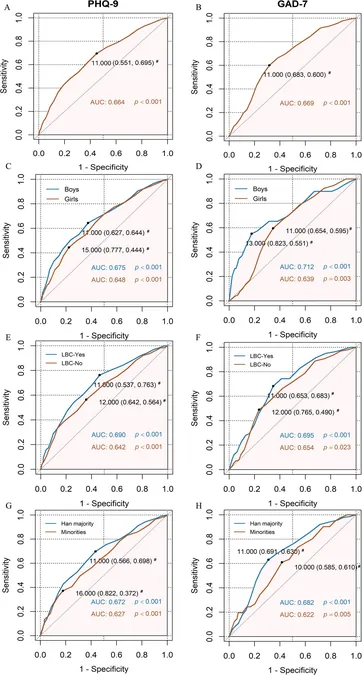
Furthermore, significant debate surrounds the appropriate cut-off scores for both scales, which is crucial for accurate screening. The commonly adopted cut-off of 10 for PHQ-9 in adults has yielded differing recommendations in youth studies, some advocating for a cut-off score of 15 instead. The GAD-7 similarly lacks consensus, with suggested cut-offs ranging from 7 to 9. These inconsistencies have created confusion among healthcare providers about optimal screening practices.
This recent study examined a large sample from an ongoing mental health survey in Yunnan Province, aiming to evaluate the discriminative abilities of PHQ-9 and GAD-7 specifically among Chinese youth while also investigating optimal cut-off scores and the influence of demographic factors on these thresholds.
Participants Involved in the Study
The sample comprised over 15,000 young individuals aged 10 to 17, sourced from a well-structured two-phase sampling approach. Schools were randomly selected, and data were collected through self-administered questionnaires followed by structured interviews with pediatric psychiatrists for those who screened positive.
Uncovering the Study Findings
The study uncovered concerning results: the AUC for both PHQ-9 and GAD-7 was below 0.7, indicative of poor discriminative ability in identifying clinical depression and anxiety. This suggests that reliance on these tools could potentially lead to misdiagnosis. Subgroup analyses revealed that various demographic characteristics—such as gender and age—greatly influenced the effectiveness of the scales. For instance, optimal cut-offs for boys and girls differed notably, emphasizing the need for tailored approaches in screening practices.
Moreover, the presence of self-harm behaviors significantly impacted the cut-off scores. Among adolescents engaging in self-harm, the required scores for positive identification of issues were higher than those for their peers without such behaviors, indicating a complex relationship between self-harm and mood disorders that warrants further exploration.
Why It Matters?
These findings illuminate the challenges of screening for mental health issues in youth populations using standardized instruments not specifically designed for them. The study highlights the importance of considering demographic factors when employing these tools, advocating for a more nuanced and culturally sensitive approach to mental health screenings in young Chinese populations.
It raises pivotal questions about the adequacy of existing screening measures and their application to diverse youth demographics. By recognizing the limitations and ensuring the application of context-specific cut-offs, mental health support systems can optimize early intervention strategies, ultimately leading to improved outcomes for affected children and adolescents.
Conclusion
This crucial examination of current practices around mental health screening among Chinese youth underscores significant imperfections in relying solely on existing tools. With alarming rates of mental health disorders among this demographic, the need for validated and reliable screening measures is greater than ever. As health professionals strive to adapt to these findings, there is an urgent call to refine detection methods and offer tailored interventions that cater to the unique landscape of youth mental health in China.
In light of these revelations, it is essential that future research continues to pave the way for improved diagnostic frameworks, with consideration for cultural and demographic nuances that shape mental health in young populations. Could the adoption of new, more effective screening tools change the mental health landscape for Chinese youth? The time to refine and innovate is now!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)