New Insights into Lung and Gut Microbiota Dynamics in Intensive Care Patients: The Hidden Connection You Need to Know!
2025-04-05
Author: Li
Introduction
In the overwhelming world of the intensive care unit (ICU), ventilator-associated pneumonia (VAP) reigns as the most prevalent hospital-acquired infection, with alarming incidence rates reaching up to 40%. This grave condition not only escalates morbidity and mortality but also imposes significant economic strains on healthcare systems. As our understanding deepens, the urgent need to explore the dynamics of the microbiota—both in the lungs and the gut—becomes clearer.
The Lung Microbiota: A Complex Community
For many years, the lungs were falsely regarded as sterile environments, but recent innovations in culture-independent microbiology have transformed this notion. We now recognize that the lung microbiota is complex and dynamic, playing an essential role in health and disease. Notably, disruptions or 'dysbiosis' within the lung microbiota can facilitate the colonization of pathogenic bacteria, leading to VAP. Furthermore, it's been demonstrated that the lung microbiota on patient admission can foreshadow clinical outcomes, including susceptibility to viral infections and the development of acute respiratory distress syndrome (ARDS).
The Gut Microbiota's Role in Critical Illness
Interestingly, the gut microbiota is intricately linked to the pathogenesis of sepsis and ARDS as well. Experimental studies have shown that gut microbiota can enhance innate immunity against infections, demonstrating the importance of this complex community in critical illness.
Research Gaps and Recent Pilot Study
Yet, despite emerging evidence suggesting a profound relationship between lung and gut microbiota in critically ill patients, understanding their simultaneous dynamics during severe illness remains a formidable challenge. Most prior research has focused on either lung or gut microbiota independently, leaving a significant gap in our knowledge regarding their interrelationship over a patient’s ICU stay.
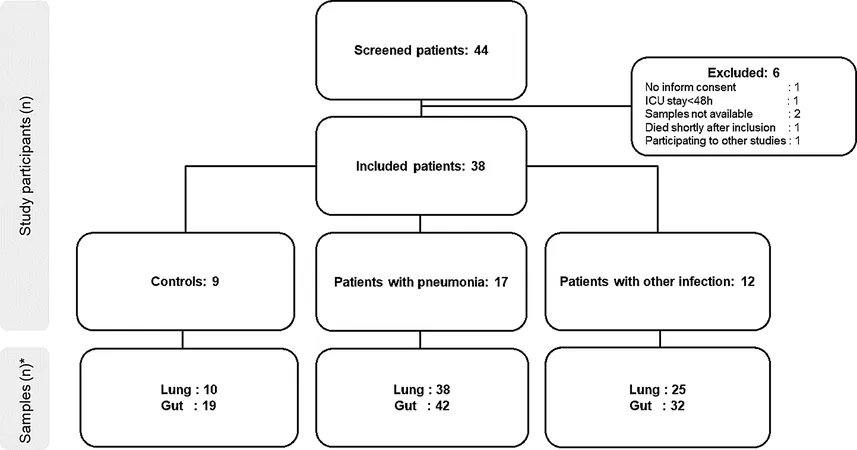
To fill this gap, a recent pilot study was conducted involving mechanically ventilated patients at the Lausanne University Hospital’s ICU. In this prospective single-center study, patients were categorized into three groups: those with ventilator-associated pneumonia (VAP), those with other infections, and uninfected control patients. This comprehensive approach allowed researchers to capture a wide array of infection-related changes in microbiota composition.
Findings from the Study
During the study, clinical, laboratory, and radiological data were meticulously collected. The analysis of longitudinal microbiota dynamics revealed notable differences in microbial alpha and beta diversity among infected and control patients. Specifically, lung microbiota diversity decreased significantly in infected patients, while the gut microbiota exhibited more resilience.
The study's findings underscored an important observation: the gut flora often serves as a reservoir for the lung microbiota, emphasizing a phenomenon known as the 'gut-lung axis.' This refers to the interaction and potential translocation of microbial communities between these two sites under critical illness conditions. For example, specific bacterial profiles—particularly an increased presence of Proteobacteria and Firmicutes—were identified in pneumonia patients, indicating a potential signature indicative of VAP.
Clinical Implications and Limitations
Furthermore, the research made noteworthy strides in establishing microbiota markers that could predict clinical outcomes. For instance, microbiome diversity measures, including the Shannon diversity index, demonstrated a negative correlation with intubation length, hinting at the potential for microbiota-based metrics to refine existing clinical scoring systems like the well-known APACHE II.
However, the study also highlights several limitations, including the necessity for larger sample sizes to validate results and the challenge of defining infections amidst the complexity of critically ill patients.
Conclusion and Future Directions
In conclusion, this pilot study sheds light on the intricate interplay of lung and gut microbiota in critically ill patients, revealing a compelling narrative that could reshape how we approach infections in the ICU. As research progresses, the hope is to leverage these microbiota insights to improve patient outcomes, highlighting the pressing need for ongoing investigations in this critical area of medicine.
Stay tuned as we continue to explore breakthroughs in microbiome research that could revolutionize our healthcare practices!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)