New Discovery: Non-Invasive Method Could Revolutionize Survival Predictions for Liver Cancer Patients!
2024-09-19
Introduction
Hepatocellular carcinoma (HCC) stands as the most prevalent type of liver cancer and ranks as the fourth leading cause of cancer-related deaths globally. For patients battling advanced stages of HCC, a range of systemic treatments, which circulate through the bloodstream to target cancer cells throughout the body, are available.
Current Treatment Practices
One notable treatment regimen is the Atezo/Bev therapy, a combination of the drugs atezolizumab and bevacizumab. This therapy is often recommended as the first line of defense for liver cancer patients. However, a significant challenge remains: the absence of reliable markers to predict how effective this treatment will be for individual patients.
Research Overview
In a groundbreaking study led by Dr. Akinobu Takaki and his team from the Department of Gastroenterology and Hepatology at Okayama University in Japan, a novel prognostic tool using anti-PD1 autoantibody was explored. Their findings, published in *Gastro Hep Advances* on August 2, 2024, offer hope for improving patient outcomes.
Key Findings
Dr. Takaki notes, “While the Atezo/Bev combination therapy exhibits considerable efficacy, nearly 20% of patients continue to show disease progression. Consequently, identifying reliable predictors of treatment efficacy is crucial for developing tailored treatment plans.”
Autoantibodies as Biomarkers
The researchers posited that autoantibodies—immune system-produced antibodies that mistakenly target an individual's own proteins—could serve as valuable biomarkers. These autoantibodies have been detected in various cancer types and are easily measurable in blood serum, making them excellent candidates for further exploration.
Focus on Anti-PD-1 Autoantibodies
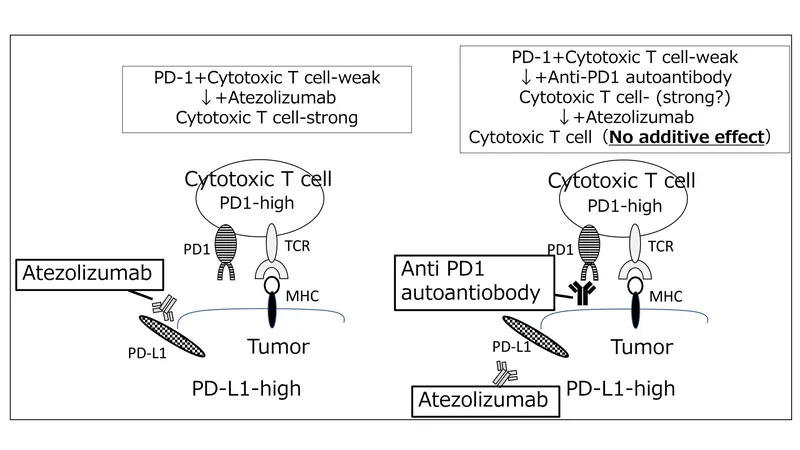
In particular, the team focused on anti-PD-1 autoantibodies, theorizing that they might influence the outcomes of Atezo/Bev therapy since they affect similar cellular pathways targeted by atezolizumab.
Study and Results
To validate this hypothesis, the team conducted a study involving 63 patients diagnosed with advanced HCC who were undergoing Atezo/Bev therapy. They measured anti-PD-1 autoantibody levels before and after treatment, analyzing the correlation between these levels and the patients' responses.
Conclusion and Future Directions
Remarkably, the results indicated a statistically significant association: higher concentrations of anti-PD-1 autoantibodies correlated with lower survival rates among patients. This suggests that anti-PD-1 autoantibody levels could serve as a promising biomarker for predicting treatment outcomes not just for Atezo/Bev but potentially for a broader range of immune checkpoint inhibitors used in treating HCC.
However, the researchers caution that further investigations are essential to fully understand the biological implications of these autoantibodies in cancer immunotherapy. This exciting discovery marks a significant step towards personalized cancer treatment, potentially transforming how physicians manage liver cancer in the future.
Final Thoughts
Is this breakthrough the key to saving more lives? Stay tuned as the research evolves!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)