Maternal Obesity: A Silent Threat to Mother and Baby? Exploring Inflammation and Oxidative Stress During Pregnancy
2025-03-13
Author: John Tan
Introduction
Recent research highlights the profound impact of maternal body mass index (BMI) on both inflammation and oxidative stress throughout pregnancy, revealing alarming insights into how obesity can disrupt the delicate balance necessary for healthy maternal and fetal outcomes. This study aimed to delve deeper into how variations in maternal BMI affect inflammatory biomarkers and dynamic thiol-disulfide homeostasis (TDH)—a critical marker for oxidative stress—during pregnancy.
Study Overview
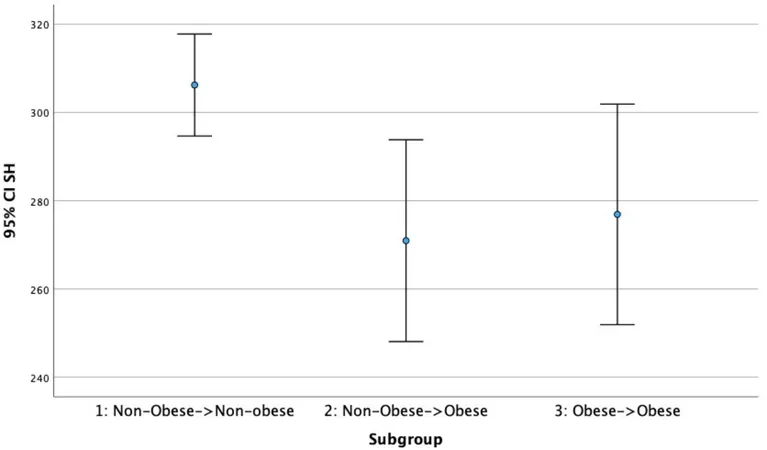
Conducted between May and June 2024 at a premier obstetric care center in Ankara, Turkey, this prospective cohort study included 125 healthy pregnant women aged over 18, who were in their late gestation period (37-41 weeks). The participants were split into three distinct groups based on their BMI before and during pregnancy: (1) non-obese both before and after (BMI < 30 kg/m²), (2) non-obese pre-pregnancy but became obese during (BMI ≥ 30 kg/m² at delivery), and (3) consistently obese (BMI ≥ 30 kg/m² from pre-pregnancy to delivery).
Maternal and fetal blood samples were collected and analyzed for levels of native thiol, total thiol, and disulfide, revealing some stark differences in the antioxidant capacities of mothers across the BMI groups.
Key Findings
The findings were startling. Those who maintained a non-obese status throughout exhibited significantly higher levels of native thiol and total thiol compared to their heavier counterparts. Specifically, the native thiol levels were an average of 306.21 μmol/L in the non-obese group, compared to lower averages in the other groups—indicative of reduced antioxidant capacity in obese mothers. Despite anticipated differences, no significant disparities concerning fetal cord blood biomarker levels were observed across the groups, suggesting potential placental compensatory mechanisms in response to maternal obesity.
This research provides strong evidence that maternal obesity disrupts thiol-disulfide homeostasis, increasing oxidative stress during pregnancy—factors known to have long-term repercussions on both maternal and fetal health.
Why Does This Matter?
The global obesity crisis is more than cosmetic; it poses serious health risks especially for women of childbearing age, as obesity is linked to a host of complications including gestational diabetes, preeclampsia, and adverse neonatal outcomes. According to the World Health Organization, nearly 1 in 8 people worldwide are obese, with troubling implications for future generations.
Past studies have shown that oxidative stress and inflammation bio-markers spike in obese individuals, potentially affecting fetal development. Disruptions in maternal antioxidant capacity not only increase the risk of complications for mothers but may also lead to long-term health issues for the offspring.
The Path Forward
Given the research findings and the pressing issue of maternal obesity, it’s crucial to initiate comprehensive interventions focusing on nutrition and lifestyle modifications for women before and during pregnancy. Importantly, weight management should be prioritized, as evidence suggests that weight loss before pregnancy can lead to significantly improved outcomes.
The present study, despite its limitations including a single-center design and potential confounding lifestyle factors, underscores the need for longitudinal studies to better understand the complexities of BMI, oxidative stress, and inflammation in pregnancy. Future research should also consider gestational weight gain patterns for a more nuanced understanding beyond BMI alone.
In conclusion, maternal obesity emerges as a silent yet formidable adversary in the realm of obstetrics, warranting immediate attention from health professionals worldwide. Understanding its impacts on maternal and fetal health is key to safeguarding the health of future generations.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)