Lung Cancer Unleashes Immune Cells to Aid Tumor Growth: New Breakthrough Revealed!
2025-09-10
Author: Siti
Groundbreaking Research Unveils Immune Manipulation by Lung Tumors
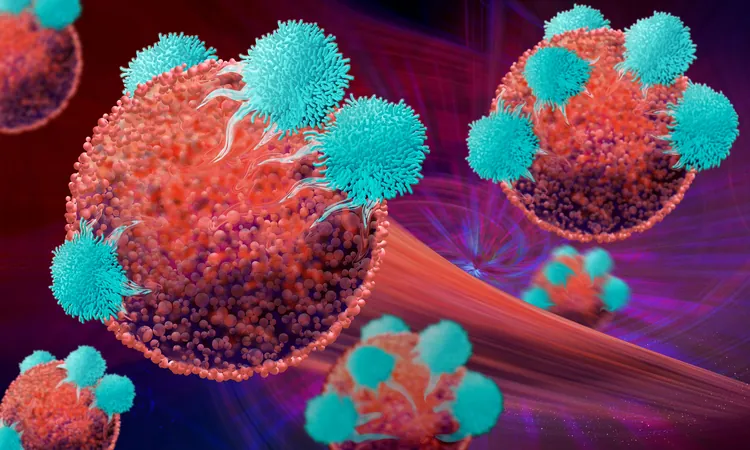
A revolutionary study from the Icahn School of Medicine at Mount Sinai has uncovered shocking insights into how lung tumors sabotage the immune system even before immune cells reach their destination. This pivotal research, now published in *Nature*, identifies an alarming two-step process that transforms myeloid progenitors—precursors of macrophages—into allies of cancer.
The 'First Hit': Early Reprogramming of Immune Cells
Lead researcher Dr. Samarth Hegde revealed that lung cancer cells send out signals that reprogram bone marrow immune cells, effectively delivering a "first hit" that weakens their ability to respond to threats. This initial alteration diminishes the interferon response, setting the stage for immunosuppression and paving the way for tumor growth.
NRF2: The Master Manipulator
Central to this manipulation is the transcription factor NRF2, a known regulator of stress responses. This study highlights its role in conditioning myeloid progenitors to adopt cancer-friendly behaviors in a hostile environment, allowing tumors to flourish unhindered. This revelation fundamentally alters our understanding of immune suppression timelines in cancer pathology.
Cutting-Edge Techniques Illuminate the Process
Utilizing sophisticated techniques such as genetically engineered mouse models and single-cell transcriptomics, researchers tracked the transition of bone marrow progenitors into tumor-associated macrophages. Their findings unveiled significant early epigenetic changes, revealing how these immune cells are prepped for a pro-cancer role long before arriving at the tumor site.
A Deadly Development: Immunosuppressive Macrophages
Once embedded in the tumor microenvironment, these macrophages take on detrimental traits, exhibiting increased oxidative stress and a decreased ability to stimulate immune responses. NRF2 activation, initiated in the bone marrow and reinforced within the tumor, is crucial in facilitating this hazardous transition.
A New Frontier in Immunotherapy
These findings could revolutionize treatment strategies for non-small cell lung cancer (NSCLC). By targeting NRF2 and disrupting the immunosuppressive cycle before it fully establishes itself, researchers aim to bolster the efficacy of existing immunotherapies. Dr. Heged emphasized the urgency of early intervention, noting that once these cells become entrenched within tumors, reversing their reprogramming may become impossible.
Promising Results from Targeting NRF2
In laboratory settings, pharmacological inhibitors like Brusatol and ML385 have demonstrated enhanced tumor control when combined with existing immunotherapy treatments such as anti-PD-1 checkpoint inhibitors. However, these successes rely on NRF2's activity in myeloid cells, as experiments on NRF2-deficient mice showed no positive effects.
Future Applications: Diagnostics and Therapeutics
The research team also sees potential for developing blood-based diagnostics capable of detecting tumor-educated immune progenitor cells, enabling early identification of immune dysregulation in NSCLC. By manipulating upstream signals like GM-CSF and IL-6, they hope to refine therapeutic strategies that hold promise for combating cancer aggression.
Exploring Broader Implications
The next steps for the team will delve into whether this NRF2-mediated reprogramming occurs in other cancers and the extensive metabolic and genetic networks that may influence this process. They will also investigate the role of extramedullary hematopoiesis in tumor-driven immune remodeling.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)