
Is a Low-Carb Diet More Effective than Medication for Managing Type 2 Diabetes?
2024-10-25
Author: Wei
Introduction
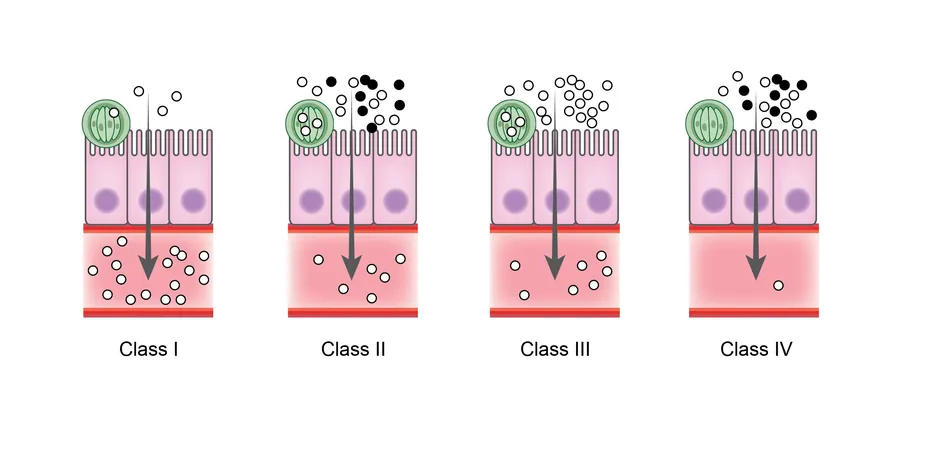
An intriguing study has emerged suggesting that individuals with mild type 2 diabetes may significantly enhance their pancreatic beta-cell function—critical cells responsible for insulin production—by switching to a low-carbohydrate diet. This finding could potentially revolutionize diabetes management and reduce reliance on medications.
The Impact of Type 2 Diabetes
Type 2 diabetes affects roughly 34 million Americans, representing about 90-95% of diabetes cases in the country. This condition arises when the insulin-producing beta cells in the pancreas become compromised, often due to excessive carbohydrate intake leading to insulin resistance. The failure in beta-cell response to blood sugar is a major factor in the progression of diabetes.
The Study
The new research, featured in the Journal of Clinical Endocrinology & Metabolism, involved a controlled trial with 57 adults aged 35 to 65 who had been diagnosed with mild type 2 diabetes within the past decade. Participants were carefully assigned to either a low-carb diet—comprising about 9% carbohydrates and 65% fats—or a higher-carb diet containing roughly 55% carbohydrates and 20% fats, all while ensuring caloric intake was maintained.
Results
Over a 12-week period, researchers examined the participants’ beta-cell function and insulin responses. Impressively, those adhering to a low-carb diet exhibited notable advancements in both initial and maximal beta-cell responses—improvements that were twofold higher and 22% greater, respectively, than their high-carb counterparts. Additionally, insulin’s capability to manage blood glucose levels improved by 32% in the low-carb group.
Racial Disparities
Notably, a remarkable disparity was noted between racial groups: Black participants on the low-carb diet demonstrated a 110% enhancement in rapid beta-cell response, while White participants showed a 48% greater improvement in maximal beta-cell response. These variances raise further questions about biological differences influencing diabetes responses and underscore the necessity for tailored dietary treatments.
Expert Opinions
Despite these impressive results, experts remain cautious regarding the long-term sustainability of low-carb diets. While they may offer immediate benefits, adherence might be challenging for some individuals. Dr. Thomas M. Holland, a physician-scientist, emphasized that a low-carb diet could alleviate the stress on beta cells by limiting glucose influx. However, not everyone with type 2 diabetes will find this dietary change suitable.
Alternative Strategies
For those not inclined towards low-carb options, several alternative strategies can effectively enhance beta-cell function. Diets such as the Mediterranean or MIND diets, which emphasize healthy fats and minimize refined carbohydrates, have demonstrated positive results. Additionally, practices like intermittent fasting, regular physical activity, and stress management can contribute significantly to improving metabolic health.
Conclusion
As promising as these findings may be, further research is vital to fully understand the relationship between diet, beta-cell function, and individual responses to dietary interventions. This study opens avenues for patients seeking non-pharmaceutical approaches to manage their diabetes and highlights the importance of personalized nutrition in diabetes care. Could this mean that adjusting our diets might be a more effective strategy than relying solely on medications? For those seeking to improve their diabetes management, this could be a game-changer!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)