How Gestational Diabetes Affects the Vaginal Microbiota: Insights from New Research
2025-03-15
Author: Rajesh
Recent research conducted at the Shenzhen Baoan Women’s and Children’s Hospital has unveiled critical insights into how gestational diabetes mellitus (GDM) influences the changes in vaginal microbiota during the perinatal period. With 51 participants selected to participate in this study, the criteria ensured that only those with full-term, singleton pregnancies free of complications were included.
The study specifically focused on women diagnosed with GDM based on oral glucose tolerance tests (OGTT) during their second trimester. Women treated strictly through diet and exercise management were selected, excluding those on medications like insulin, to avoid skewing the results regarding vaginal microbiota alterations.
Sample Collection and Analysis
Vaginal secretions were meticulously collected at three key time points: one week before delivery (D0), on the day of delivery (D1), and 42 days postpartum (D42). Researchers employed sterile procedures to obtain these samples, ensuring that they accurately represented the vaginal microbiota during these critical phases.
The DNA from these samples was then analyzed using advanced sequencing techniques, focusing on the 16S rRNA gene which is pivotal for classifying prokaryotic organisms. This allowed the researchers to assess the diversity of bacterial communities through various bioinformatics tools and methodologies.
Key Findings on Microbial Changes
The analysis revealed significant shifts in the vaginal microbiota. Contrary to what one might expect regarding GDM's adverse effects, both GDM and non-GDM groups showed overlapping microbial communities across the three time frames. However, the changes within the GDM group indicated a notable decrease in Lactobacillus — a genus crucial for maintaining vaginal health.
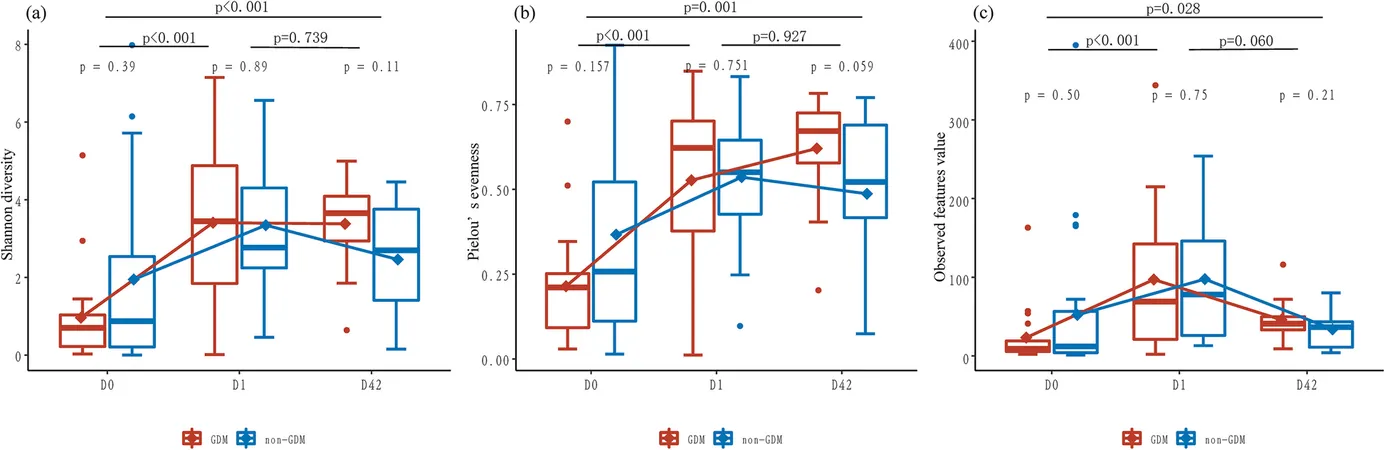
While the overall diversity (alpha diversity) metrics between the GDM and non-GDM groups were not significantly different, the dynamics of microbial populations varied over time, with the GDM group experiencing a more pronounced decline in Lactobacillus following childbirth. This decline is concerning, as lower Lactobacillus levels are often correlated with increased susceptibility to infections and conditions such as bacterial vaginosis (BV).
Implications for Postpartum Health
The research highlighted that postpartum hormonal shifts, alongside the bacterial transitions, could contribute to potential vulnerabilities in the vaginal ecosystem. Notably, after delivery, many women’s vaginal microbiota began to shift towards types of bacteria commonly associated with BV.
The study also pointed out that certain metabolic pathways were more active in the GDM group postpartum, indicating that there might be a diverse array of microbial metabolites present that could have unclear effects on overall health.
Recommendations Moving Forward
Given the research findings, it is essential for health practitioners to remain vigilant regarding the vaginal health of women with a history of GDM. The significant reduction in protective bacteria post-delivery in this group suggests they may benefit from probiotic supplements to restore balance to the vaginal microbiota and potentially avert infections.
Moreover, the study emphasizes the need for larger sample sizes in future research and more extensive longitudinal studies to understand better the long-term implications of these microbiota changes on women's health post-pregnancy.
Conclusion
The study provides a critical leap towards understanding how gestational diabetes can influence vaginal microbiota dynamics during vital periods. As our knowledge evolves, it is imperative to refine postpartum care strategies for women with GDM, potentially utilizing probiotics to bolster vaginal health and prevent infections, thereby promoting healthier outcomes for both mothers and infants.
This groundbreaking research opens up avenues for future studies, especially in exploring possible interventions to maintain vaginal equilibrium in the context of GDM and beyond.
By addressing these gaps, we can enhance our understanding of how metabolic conditions like gestational diabetes impact broader aspects of women's health, paving the way for improved medical guidance and care practices.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)