How COVID-19 Changed the Game for HIV Prevention in Uganda: Shocking Findings Revealed!
2024-11-12
Author: Sarah
Background
As the world grappled with the COVID-19 pandemic, Uganda faced unique challenges in preventing mother-to-child transmission of HIV (PMTCT). The lockdown measures in April to June 2020 imposed severe restrictions, including banning public transport and requiring pregnant women to obtain travel permits. These restrictions deeply affected PMTCT services, prompting innovative adaptations like community drug delivery and home-based DNA-PCR testing for HIV-exposed infants (HEI). This article delves into the impact of these pandemic-induced changes on PMTCT service uptake in Central Uganda.
The Methods
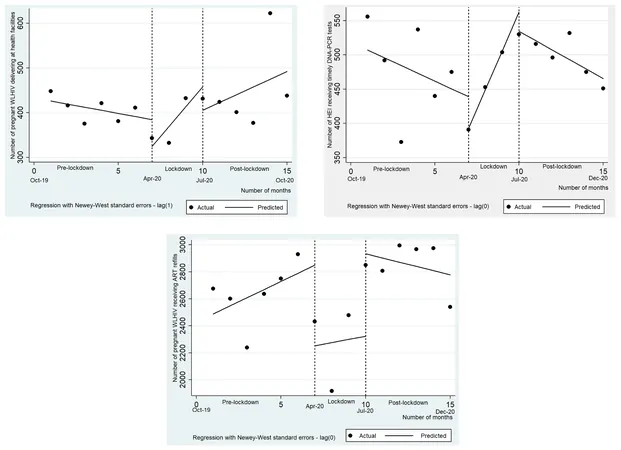
Data from pregnant women living with HIV and their infants were meticulously analyzed across eight districts in Central Uganda. By comparing data from the six months prior to the lockdown (October 2019 - March 2020), the lockdown period itself, and the six months that followed, we were able to uncover trends in service uptake. Key indicators included monthly antiretroviral therapy (ART) refill attendance, health facility deliveries, and timely DNA-PCR testing for HEI. Using segmented ordinary least squares regression, we adjusted for fluctuations in service uptake.
Results: A Tale of Two Halves
In October 2019, when life was "normal," there were 448 deliveries, 2,676 ART refills, and 556 timely HEI tests across the clinics studied. However, as Uganda entered lockdown, all service uptake plummeted, with facility deliveries dropping by a staggering 60. Surprisingly, during the lockdown, innovative adaptations allowed for a revival in some areas—both HEI testing (up by 68 tests monthly) and deliveries (increasing by 51) saw positive trends before hitting another snag post-lockdown.
After the lockdown ended, HEI testing numbers nosedived with 70 fewer infants tested per month. Disturbingly, while deliveries and ART refill rates remained somewhat stable, they failed to fully recover to pre-lockdown levels.
Chilling Reality of Health Worker Strain
The onset of the pandemic wasn't just hard on pregnant women; health workers also felt the brunt. Fears of contracting COVID-19, coupled with lack of PPE and resources, led to increased absenteeism among healthcare providers. Some pregnant women avoided facilities entirely, opting instead to rely on traditional birth attendants or to give birth at home—conditions that significantly increased the risk of HIV transmission to their infants.
Innovative Program Adaptations
Despite these challenges, Uganda’s PMTCT program adapted significantly. Transport facilitation for healthcare workers and the introduction of multi-month ART refills allowed pregnant women living with HIV to access the medication they needed without the monthly trips to the clinic that had previously been mandated. This flexible approach proved essential during such unprecedented times.
Implications for the Future
The findings highlight a crucial need: as Uganda continues to navigate the complexities of the post-pandemic world, maintaining the successful adaptations implemented during the lockdown is vital. Implementing support systems for pregnant women living with HIV, ensuring access to ART, and continuing home testing for infants could restore and even enhance progress toward eliminating mother-to-child HIV transmission.
Key Takeaways
While the COVID-19 pandemic introduced severe setbacks in PMTCT services across Central Uganda, the rapid adaptations made in response reveal a resilience and an opportunity to rethink and enhance care protocols. As we emerge from the shadows of COVID-19, addressing these lessons and adapting them into standard practice could prevent a potential backlash in the fight against HIV transmission to newborns.
The road ahead remains challenging, but with strategic interventions and sustained innovation, Uganda has the potential to rebound stronger than before. Will these changes persist, shaping a new future in healthcare? Only time will tell!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)