Hidden Dangers: The Overlooked Risk of Latent Tuberculosis in Rheumatic Patients
2025-09-02
Author: Arjun
Tuberculosis: A Persistent Global Threat
Despite medical advances, tuberculosis (TB) remains a formidable global health challenge, ranking among the deadliest infectious diseases. Upon infecting individuals with Mycobacterium tuberculosis (MTB), a subset may swiftly develop active TB, while many enter a prolonged latent phase known as latent tuberculosis infection (LTBI). This condition sees individuals harboring TB without showing active disease, thus acting as a potential reservoir for future infections.
The Alarming Scale of Latent TB
As of 2018, nearly one-third of the global population was estimated to have been infected with MTB, with China alone reporting over 200 million cases of LTBI by 2021. While LTBI itself isn't contagious, the prospect of it evolving into active TB is heightened in immunocompromised individuals, including those suffering from various rheumatic diseases.
Rheumatic Diseases and Their Connection to TB Risk
Rheumatic diseases like rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), and scleroderma, which predominantly affect the body’s connective tissues, present unique challenges. These conditions often involve immune dysregulation, which may increase susceptibility to infections, including LTBI. Research shows that patients with RA and SLE have heightened immune responses coupled with impaired defenses against TB.
Breaking Down the Risk Factors for LTBI
Recent studies have uncovered various risk factors for LTBI specifically in rheumatic patients. Current smoking has been identified as a significant risk, increasing the likelihood of LTBI by 50%. Anti-TNF therapy, particularly Golimumab, also raises risks, while a history of TB correlates with a staggering threefold increase in developing LTBI.
Who is at Highest Risk?
Men tend to be more affected, with studies indicating a 72% higher risk in males compared to females. Age over 40 similarly contributes to increased susceptibility, as does the use of Chloroquine—a common treatment for rheumatic diseases that may impair the immune system's ability to combat infections.
The Disturbing Prevalence of LTBI in Rheumatic Populations
In a review of over 12,000 rheumatic patients, a sobering 22% were found to have LTBI. This prevalence underscores a critical need for proactive screening and preventive measures in this vulnerable population.
Important Implications for Care
Understanding these risk factors is vital for rheumatologists and other healthcare professionals. With various treatments potentially exacerbating susceptibility to TB, careful monitoring and tailored preventive strategies are crucial for managing these patients.
Towards Better Outcomes
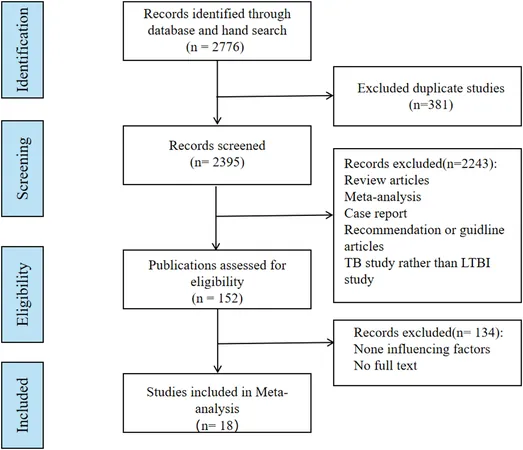
This meta-analysis aims to fortify the evidence base for recognizing LTBI risks in rheumatic patients. By addressing these links, healthcare providers can take proactive steps, ensuring better patient outcomes and potentially saving lives.
A Call to Action
In light of these findings, there is an urgent need for heightened awareness and targeted screening for LTBI within rheumatic disease populations. As we confront the global TB dilemma, understanding and mitigating the risks for our patients is more important than ever.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)