Gut-First Approach: New Findings on Parkinson's Disease Linked to Gut Dysbiosis
2024-10-24
Author: Wei Ling
What Is Dysbiosis and How Does It Affect Parkinson’s Disease?
Dysbiosis refers to an imbalance in the microbial community within the gut that can affect health. In patients with Parkinson's disease, altered gut microbiomes could potentially exacerbate motor and cognitive symptoms, as suggested by various studies emphasizing this connection.
In a comprehensive study, fecal samples were obtained from patients at the Movement Disorders Unit of the Centro Hospitalar e Universitário de Coimbra. The participants included individuals diagnosed with idiopathic PD who were over 50 years old and experienced symptoms suggesting constipation. The control group was similarly aged but free from neurological disorders.
Through fecal microbiota transplantation (FMT) in mice, researchers aimed to understand the precise impact of gut dysbiosis on the progression of PD. This involved colonizing wild-type male C57BL/6 mice with fecal matter from both PD patients and healthy individuals. The results were alarming—mice that received microbiomes from PD patients exhibited notable motor deficits and a reduction in dopaminergic neurons, highlighting the contribution of the microbiome to the pathology of PD.
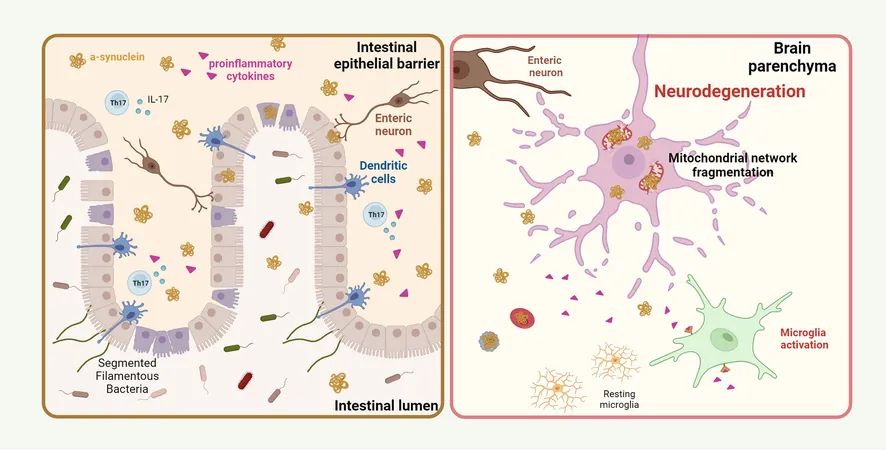
The Science Behind It: How the Gut Affects the Brain
Study methods included a series of clinical trials with blood and ileal biopsies, analyzing microbiome profiles and assessing the neurobehavioral performance of the mice. It was discovered that the transplanted microbiota from PD patients significantly impacted motor behavior, indicating the real and pressing influence of gut health on brain function.
The methodology included advanced sequencing techniques to analyze microbial DNA alongside behavioral assessments designed to measure anxiety and memory, thus providing a holistic view of how gut bacteria can affect coordination and cognitive functions.
Gut Inflammation: A Catalyst for Neuroinflammation
Upon transplanting PD-associated microbiota, researchers observed various inflammatory markers in the mice. This inflammatory response likely triggered an erosion in the gut's mucosal layer, leading to a weakened intestinal barrier. The implications suggest that mice with such gut dysbiosis also showed increased levels of pro-inflammatory cytokines like TNF-α and IL-17, correlating with systemic inflammation.
Moreover, the study found that this pro-inflammatory state is linked to a loss of structural integrity in tight junction proteins such as ZO-1, which are crucial for maintaining intestinal barrier function. As the barrier weakens, it allows for the infiltration of harmful substances, further fueling neuroinflammation and potentially leading to dopamine neuron loss.
The Bigger Picture: Implications for Treatment
These research findings underscore the necessity of a "gut-first" approach in understanding and treating Parkinson's disease. With gut health at the forefront, therapeutic strategies could revolve around dietary interventions and microbiome modulation to restore balance in the gut flora and, consequently, improve neurological health.
As scientists continue to unravel the intricacies of how the gut impacts the brain in conditions like PD, potential preventive measures and innovative treatments may arise, paving the way for enhanced quality of life for patients.
Clickbait Conclusion: Are You Ignoring This Hidden Link? Discover How Your Gut Health Could Be Tied to Parkinson's Disease!
In essence, the connection between gut dysbiosis and Parkinson's disease opens new avenues for research and treatment, emphasizing that maintaining gut health could be critical not only for digestive wellness but also for protecting against neurodegeneration.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)