Groundbreaking Study Reveals Two Distinct Molecular Subtypes of Crohn’s Disease—What It Means for Future Treatments!
2024-09-27
Crohn's disease, a complex autoimmune disorder, wreaks havoc on the digestive tract, resulting in chronic inflammation and a range of distressing gastrointestinal symptoms that can severely impact quality of life. This elusive condition, which has no known cure and limited treatment options, predominantly affects young individuals, forcing them to endure a lifetime of discomfort. One of the significant challenges in treating Crohn’s disease is its considerable variability among patients, making tailored therapies difficult to establish.
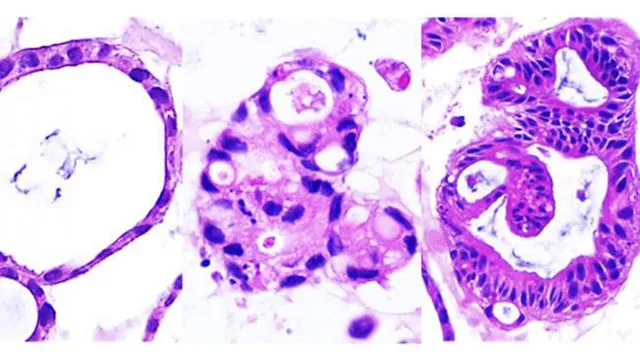
In a groundbreaking study conducted by researchers at the University of California San Diego, an exciting leap forward has been made in understanding Crohn's disease at the molecular level. By utilizing organoids—miniature, lab-grown replicas of human organs derived from adult stem cells in the gut tissue of Crohn's patients—the researchers discovered that the disease comprises two distinct molecular subtypes. These findings, published in Cell Reports Medicine on September 26, 2024, could pave the way for more precise diagnostics and personalized treatment strategies.
The research involved gut tissue samples from 53 Crohn's disease patients undergoing routine colonoscopies at UC San Diego's Inflammatory Bowel Disease Center. The diverse selection of patients, each with varying clinical symptoms, enabled the scientists to create a comprehensive “biobank” of patient-derived organoid cultures. Lead researcher Dr. Courtney Tindle noted that the adult stem cells used in this study retain an “epigenetic memory” of the gut environment, offering a more accurate representation of the disease than previous models developed from pluripotent stem cells.
Two Unique Subtypes of Crohn's Disease
Upon further investigation, the team identified two unique subtypes of Crohn’s disease: 1. Immune-Deficient Infectious Crohn’s Disease (IDICD): This subtype is marked by an ineffective immune response, resulting in difficulties in clearing pathogenic infections and frequent fistula formation. 2. Stress and Senescence-Induced Fibrostenotic Crohn’s Disease (S2FCD): Patients with this subtype experience cellular aging and stress, leading to scarring (fibrosis) of the gut tissue and potential strictures.
Dr. Pradipta Ghosh, the senior author of the study, emphasized a significant shift in understanding Crohn's disease could arise from these findings. Instead of treating all patients with a generalized "one-size-fits-all" approach, recognizing these molecular subtypes could revolutionize treatment strategies, enabling more targeted interventions.
“Currently, treatment regimens largely consist of anti-inflammatory medications, which only address symptoms temporarily,” Ghosh pointed out. “The identification of these two subtypes suggests that therapies should be more specialized—IDICD patients might benefit from treatments aimed at managing infections, while S2FCD patients could see improvements from therapies that target cellular aging.”
The potential for personalized therapies aligns with the larger shift in medicine towards customized patient care. Future strategies may include innovative treatments such as gene editing or RNA-based therapies tailored to the specific molecular characteristics of an individual’s Crohn's disease subtype.
As ongoing research continues, the team plans to genotype the two identified subtypes to develop rapid testing methods for precise diagnosis. Dr. Ghosh is hopeful that their findings will transform the management of Crohn’s disease for the over 500,000 affected Americans, offering renewed hope to those who have long awaited better therapeutic options.
Stay tuned for more updates on this revolutionary study that could change the landscape of Crohn's disease treatment forever!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)