Groundbreaking Study Reveals Survival Insights for Men Who Have Sex with Men Living with HIV in Southern China: A 10-Year Analysis!
2025-01-28
Author: Yu
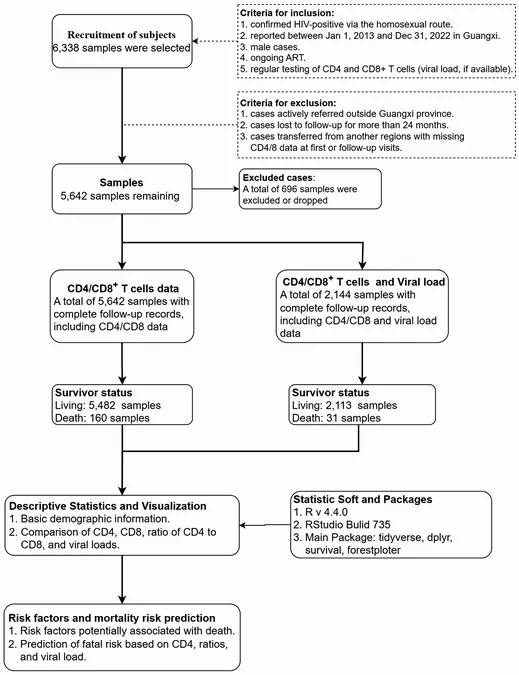
Study Design and Population
The research utilized data from the China HIV Antiretroviral Treatment Management System, involving 112 ART-treating hospitals in Guangxi. This retrospective cohort analysis included 5,642 MSM with HIV who had begun ART between January 1, 2013, and December 31, 2022. To ensure reliability, participants must have met specific criteria such as being male, receiving regular follow-up care, and having available immunological data, specifically CD4+ and CD8+ T cell counts. Participants faced exclusion if they were transferred to other provinces, lost to follow-up for over 24 months, or had incomplete records. The study aimed to track the survivability and health trends of these patients to generate insights that can enhance HIV treatment and management strategies.
Demographics and Findings
Among the participants, the leading demographic characteristics revealed that the majority were aged 20–29 years, educated at least to college level, and primarily unmarried. By March 31, 2023, during the follow-up period, 160 deaths were recorded, leading to a mortality rate of 2.8%. Notably, the median age of survivors was 32.7 years, compared to 37.3 years for those who unfortunately passed. The findings highlighted significant differences in mortality related to various factors such as age, occupation, and immunological markers. Particularly alarming was that 66.6% of participants were at WHO stage 1 at diagnosis, revealing the importance of early detection and treatment.
Immunological Indicators: A Revelation
The study investigated several immunological indicators: CD4+ T cell counts, CD8+ T cell counts, and the CD4+/CD8+ T cell ratio. The results indicated that surviving patients had better immunological profiles than those who did not survive. For instance, the median CD4+ T cell counts increased significantly among survivors, contrasting sharply with lower counts in deceased individuals. Additionally, the analysis of viral load revealed that while many patients showed substantial reductions in viral load over time, those who had counts exceeding 100,000 copies/mL faced drastically lower survival probabilities—their prognosis was particularly severe.
Survival Curves and Risk Factors
Utilizing Kaplan-Meier (K-M) survival curves, researchers noted that patients aged 60 and above had significantly reduced survival probabilities compared to younger counterparts. The study identified several risk factors that contributed to a higher likelihood of mortality, including age, baseline CD4+ T cell counts below 200 cells/µL, and unfavorable CD4+/CD8+ T cell ratios.
Implications for Future Care and Research
The results of this pivotal study offer critical insights into the management of MSM living with HIV. The ability to pinpoint high-risk factors allows healthcare providers to tailor interventions more effectively, ultimately aiming to reduce mortality rates within this population. Continuous education, improved access to ART, and regular health monitoring—including viral load testing—are paramount. However, the study does have limitations. The relatively low mortality rate may not provide a comprehensive view of long-term clinical outcomes, and variations in ethnic minority representation could impact the generalizability of the findings. In conclusion, this landmark study not only underscores the impressive advancements in HIV treatment but also emphasizes the necessity for tailored healthcare strategies to maximize survival outcomes for vulnerable populations. Future research will focus on addressing existing gaps and improving care for MSM living with HIV in Southern China and beyond.
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)