Groundbreaking Study Reveals No Direct Connection Between Osteoarthritis and Cognitive Decline – but Here's What You Need to Know!
2025-01-25
Author: Jia
Study Overview
A recent study published in *Therapeutic Advances in Musculoskeletal Diseases* has refuted the notion of a direct link between osteoarthritis (OA) and cognitive decline. Surprisingly, the study suggests that depression may be a significant mediator influencing mental outcomes in individuals with OA.
Research Methodology
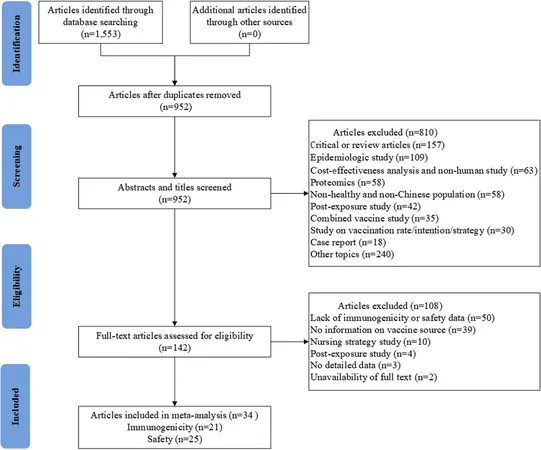
The researchers examined the relationship between OA and cognitive impairments by analyzing past studies that have often been criticized for bias due to confounding factors and reverse causality. Their goal was to clarify these associations and investigate potential causal relationships.
The research was conducted in two key stages. The first utilized data from the National Health and Nutrition Examination Survey (NHANES), which is a comprehensive assessment of the health and nutritional status of American civilians. The study focused on participants aged 60 and older who had completed cognitive function tests, while also gathering OA status information. This method allowed the researchers to use sophisticated statistical techniques to ensure that their findings were representative of the broader population.
During the second stage, a two-sample Mendelian randomization (MR) analysis was employed to assess the causal links between OA (including knee and hip OA) and various dementia subtypes. MR is a powerful statistical technique that relies on genetic variants as instrumental variables, thereby reducing bias from confounding factors.
Study Findings
In total, the study involved 2,199 participants, representing an estimated 42.5 million individuals in the U.S. Among them, 709 had OA, and 1,490 did not. The findings were intriguing: despite higher rates of depression (9.78%) and larger body mass index (BMI) in individuals with OA, there were no significant differences in cognitive performance measurements, including word recall and animal fluency, between the two groups.
However, when the data was further dissected, the study revealed a striking association between depression and lower cognitive performance in total word recall. In fact, individuals with depression were nearly five times more likely to exhibit poor word recall abilities. Additionally, being female was correlated with poorer performance in animal fluency tasks.
Mendelian Randomization Analysis
The MR analysis did not find significant causal links between OA and dementia, Alzheimer's disease, or vascular dementia. Interestingly, it did suggest that major depression could mediate the relationship between OA and vascular dementia, indicating a complex interplay between these conditions.
Conclusion and Implications
The authors of the study highlighted an important takeaway: “There is no significant association between OA and cognitive decline when adjusting for relevant covariates,” affirming the need for further investigation into the connections between OA, depression, and cognitive impairment. They called for future studies to explore these relationships, which could eventually lead to targeted interventions aimed at preventing cognitive decline in those suffering from OA.
This research provides vital insight, suggesting that while osteoarthritis itself may not lead directly to cognitive decline, the emotional and psychological burdens associated with the condition, such as depression, can indeed impact cognitive health. As we strive to understand these intricate relationships, further exploration could illuminate new pathways for interventions and improve quality of life for millions living with osteoarthritis.
Stay Informed
Stay tuned for more updates on health research that can make a difference in your life!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)