Groundbreaking Study Reveals How Therapeutic Hypothermia Can Save Lives After Heart Attacks and Cardiac Arrests!
2025-03-26
Author: Mei
In recent years, therapeutic hypothermia has emerged as a promising treatment for patients suffering from acute myocardial infarction (AMI) who also experience out-of-hospital cardiac arrest (OHCA). Despite the potential benefits, there has been limited data on its effectiveness prior to a recent extensive study aiming to bridge this gap.
Understanding the Study
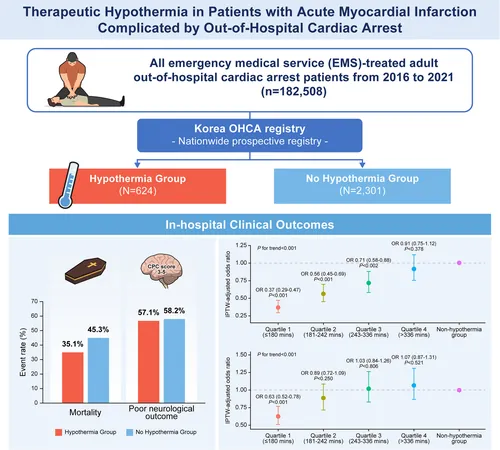
Conducted using a nationwide registry from 2016 to 2021, this breakthrough study analyzed data from 2,925 patients who underwent emergency percutaneous coronary intervention (PCI) for AMI after experiencing OHCA. The patients were categorized into two groups: those who received therapeutic hypothermia (624 patients) and those who did not (2,301 patients). Researchers primarily focused on in-hospital mortality rates while also evaluating secondary endpoints like mortality rates after 24 hours and neurological outcomes at discharge.
Key Findings
The results were compelling. The hypothermia group exhibited a significantly reduced in-hospital mortality rate, with an odds ratio of 0.71 (confidence interval: 0.59–0.85; P < 0.001), compared to their non-hypothermia counterparts. Surprisingly, however, no substantial difference was observed in neurological outcomes between the two groups. This indicates that while hypothermia can be lifesaving, it does not necessarily enhance cognitive recovery post-event.
A notable aspect of the study was the analysis of the "door-to-cooling" (DtC) time, which is the interval from hospital arrival to the initiation of hypothermia. Findings showed that shorter DtC times were associated with a marked decrease in both mortality and poor neurological outcomes, suggesting that timely intervention is crucial. For instance, those who received hypothermia within 180 minutes had a 40% lower mortality risk than those whose treatment was delayed.
Implications for Future Treatments
The implications of these findings are enormous. They suggest that therapeutic hypothermia should not only be considered as a vital treatment option but also that the speed at which it is administered can greatly influence patient outcomes. Emergency medical teams and hospitals now have even more incentive to establish rapid protocols for initiating hypothermia in at-risk patients.
Moreover, the discussion about the specific parameters of hypothermia, like the target temperature (33 °C vs. 36 °C) and the duration of therapy (24 hours vs. 48 hours), revealed no significant differences concerning mortality rates or neurological recovery. This means that further research is needed to refine treatment protocols and discover the optimal conditions for therapeutic hypothermia.
Challenges and Future Research
Despite the promising outcomes, the study faced limitations such as a non-randomized design, potential biases, and limited available data on various patient traits. Future investigations must address these gaps, focusing on long-term outcomes and the economic impacts of hypothermia treatments.
Conclusion
In summary, this landmark study offers strong evidence supporting the use of therapeutic hypothermia for reducing in-hospital mortality in AMI patients who suffered OHCA, stressing the need for prompt treatment. As new research progresses, the hope is to not only enhance survival rates but also improve the quality of life for survivors in a meaningful way. Can therapeutic hypothermia become the golden standard for emergency cardiac care? Only time—and further research—will tell!
Stay tuned as we monitor advancements in cardiac arrest treatments, keeping you informed about the latest and most effective options available in our fight against heart disease!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)