Groundbreaking Research Links Immune Cells in the Brain to Depression
2025-09-01
Author: Wei
Shocking New Findings on Depression and the Immune System
Recent research has unveiled a surprising connection between immune cells and mental health, suggesting that these cells may contribute significantly to depression and anxiety symptoms. Scientists at the University of Cambridge and the National Institute of Mental Health conducted a study on mice that reveals how chronic stress can trigger immune responses in the brain, reshaping our understanding of mood disorders.
The Hidden Epidemic of Mood Disorders
Did you know that around 1 billion people will experience a mood disorder like depression or anxiety in their lifetime? While numerous factors can contribute to these conditions, chronic inflammation has emerged as a significant player. It’s when the immune system remains on high alert for extended periods—even in the absence of an infection—that it may drive mental health issues, suggesting a possible solution lies in understanding the immune system’s role.
Neutrophils: The Culprits Behind Depression?
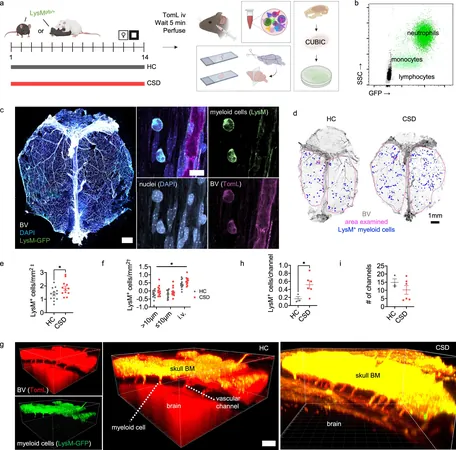
Previous studies hinted at the involvement of neutrophils, a type of white blood cell, in the severity of depression. But their exact impact remained unknown until this groundbreaking study analyzed how stress affects these cells. The research indicated that enduring stress might result in the release of neutrophils from bone marrow located in the skull, which then migrate to the meninges—the protective membranes surrounding the brain—leading to depressive symptoms.
Chronic Stress Unleashes Immune Responses in Mice
In an innovative experiment, researchers exposed mice to chronic social stress by introducing an 'intruder' mouse into the cage of an aggressive resident. This stress-induced environment triggered a spike in neutrophil levels within the meninges, which correlated with behavioral changes typical of depression. Surprisingly, these immune cells lingered even after the stress was removed, which was not the case in the bloodstream.
A Potential Breakthrough in Treatment Methods
The findings from this study pave the way for new treatment avenues focusing not just on brain chemistry but also on the immune system. Dr. Stacey Kigar from the Cambridge team emphasized that this research opens doors for innovative therapies designed to manage depression more effectively, particularly for the estimated one in three patients who find traditional antidepressants ineffective.
Decoding the Meningeal Mystery
But what exactly causes neutrophils to congregate in the meninges? One theory posits that microglia, the brain's specialized immune cells, recruit these neutrophils. Another possibility is that stress-induced microhemorrhages—tiny breaches in blood vessels—attract neutrophils to the damaged areas, inadvertently causing further brain inflammation as they get trapped.
The Connection Between Immunity and Mood
Dr. Mary-Ellen Lynall stated that while the link between immune responses and depression has long been suspected, the mechanisms were unclear. Their research not only confirmed the movement of these immune cells from the skull to the brain but also illuminated how chronic immune activation can lead to prolonged mood disturbances.
A Potential Path to Personalized Treatments
The discovery may also provide a biomarker to identify patients whose mood disorders stem from inflammation. This could enhance the effectiveness of future clinical trials, ensuring that new drugs targeting inflammation reach the patients who truly need them, ultimately improving treatment success rates.
Final Thoughts: A New Era in Understanding Mental Health
As we delve deeper into the intricate relationship between our immune systems and mental health, this groundbreaking research offers hope for millions battling mood disorders. Understanding the immune system's role could herald a new era in the treatment of depression and anxiety, paving the way for more personalized and effective therapies.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)