Groundbreaking Research Connects Gut Health and Hypertension: A Path to Revolutionary Blood Pressure Treatments!
2025-01-29
Author: Wei
In an exciting development, researchers at Monash University have unveiled crucial insights into how our gut health and dietary choices influence high blood pressure. This groundbreaking study could lead to the creation of targeted new medications aimed at treating hypertension, a condition affecting approximately one in three Australians and a major contributor to heart disease, strokes, and kidney complications.
Research Team and Focus
Led by Professor Francine Marques at the Hypertension Research Laboratory, the research team comprised experts from Australia, China, and Singapore. Their findings focus on the relationship between dietary fiber intake and blood pressure regulation, revealing that certain gut-produced substances could be the key to unlocking better treatment options.
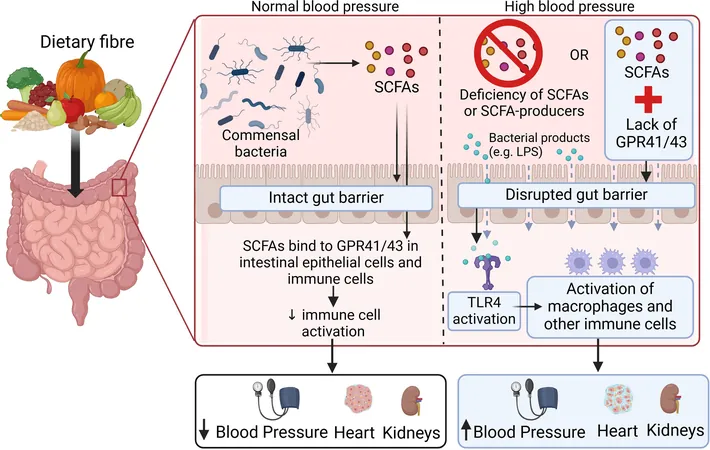
“Previous evidence suggested that dietary fiber—specifically through the generation of short-chain fatty acids by gut microbes—has a blood pressure-lowering effect,” explained Professor Marques. However, the precise mechanism behind this gut-to-host communication was previously unclear.
Discovery of Protein Receptors
The researchers identified two protein receptors, GPR41 and GPR43, that reside in intestinal cells and are activated by short-chain fatty acids. “These receptors are part of the largest group of receptors known to maintain cell signaling,” states Professor Marques. “They are highly concentrated in immune and intestinal lining cells, where their activation can spur anti-inflammatory responses.”
As we consume fiber-rich foods—such as legumes, fruits, vegetables, nuts, whole grains, and resistant starches—gut microbes ferment this fiber, producing beneficial short-chain fatty acids. Sadly, many Australians fall short of the recommended fiber intake, which poses a significant health risk.
Gut Permeability and Inflammation
The team's findings, recently published in *Circulation Research*, highlight gut permeability—a condition in which the gut lining becomes "leaky." Dr. Rikeish R Muralitharan, the lead author of the study, notes, “When fiber intake is insufficient, receptor activation declines, resulting in increased gut permeability that lets microbial components enter the bloodstream.” This, in turn, triggers inflammation in vital organs such as the kidneys, which play a pivotal role in regulating blood pressure.
Genetic Insights
Remarkably, the research also analyzed genetic data from around 300,000 individuals, revealing that specific genetic variants correlate with reduced hypertension rates. This important link suggests that our genetic makeup may influence individual responses to fiber intake and blood pressure regulation.
Future Directions
To further advance this groundbreaking work, Professor Marques's laboratory is embarking on a human clinical trial aimed at elucidating gut permeability's role in hypertension. They are also engaging in laboratory tests to develop potential new medication that activates the GPR41 and GPR43 receptors, signaling a promising new avenue for hypertension treatment.
“By collaborating with specialists in computational drug discovery, we hope to design and test innovative drugs that target these receptors,” said Marques. “This could revolutionize the way we approach blood pressure management, leveraging gut biology to improve patient outcomes.”
Conclusion
With these strides in our understanding of the gut’s impact on hypertension, the future could hold a new chapter in the fight against high blood pressure—one where simple dietary changes and groundbreaking new treatments work hand-in-hand for better cardiovascular health!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)