Groundbreaking MyeloMATCH Initiative Aims to Transform Treatment for Acute Myeloid Leukemia
2024-09-20
Author: Mei
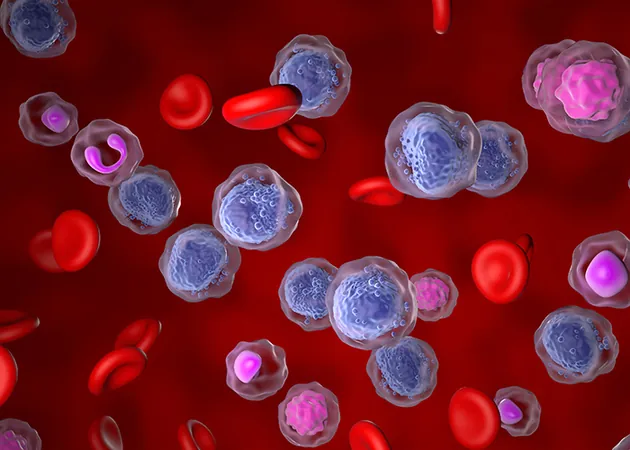
In a bold step towards revolutionizing cancer treatment, the National Cancer Institute has launched an ambitious precision-medicine initiative aimed at tackling acute myeloid leukemia (AML), the most prevalent type of acute leukemia in adults. This aggressive disease sees the bone marrow producing abnormally high levels of dysfunctional blood cells and currently boasts a stark five-year survival rate of only 30%.
Enter MyeloMATCH (Myeloid Malignancies Molecular Analysis for Therapy Choice) — a groundbreaking “umbrella trial” encompassing a series of clinical substudies focused on individuals diagnosed with either AML or myelodysplastic syndrome (MDS). MDS, often considered a precursor to AML, is marked by a shortage of healthy blood cells, further complicating patient outcomes.
With over 100 participating sites nationwide, MyeloMATCH represents the largest concerted effort in the U.S. aimed at addressing these difficult-to-treat myeloid cancers, incorporating innovative treatment trials and protocols from prominent cancer research groups, including the Alliance for Clinical Trials in Oncology and SWOG Cancer Research Network.
“This initiative marks a pivotal moment for the U.S. leukemia community,” stated Dr. Tara Lin, director of the adult leukemia program and principal investigator for MyeloMATCH at The University of Kansas Cancer Center. “It has taken time to develop, but we’re finally seeing it recognized as a national priority.”
The multisite trial, which commenced this summer at the KU Cancer Center and Masonic Cancer Alliance institutions, is enrolling individuals aged 18 and older who may have AML or MDS. Patients will undergo screening at diagnosis for specific biomarkers found in their blood and bone marrow, such as gene mutations and proteins. This data is crucial for assigning patients to specific substudies targeting their unique genetic profiles.
Notably, MyeloMATCH promises expedited results, delivering diagnostic information in just 72 hours—a significant decrease from the traditional weeks-long wait. “This rapid access to diagnostic information is something we simply haven’t had before,” emphasized Lin.
For patients without available substudies at diagnosis, standard care will still be provided, but they will remain in MyeloMATCH’s care framework, potentially qualifying for later trials as their disease progresses.
Dr. Lin is also co-leading a substudy aimed at patients under age 60 with high-risk AML. This trial will compare newer experimental treatment regimens, using a combination of additional drugs against the established standard-of-care, with the goal of boosting the number of patients achieving minimal residual disease (MRD) negativity. Achieving MRD negativity indicates a lower number of remaining cancer cells and is seen as a strong predictor of long-term survival.
Additionally, another MyeloMATCH substudy is assessing the effects of introducing an innovative drug for older patients displaying the most common mutation seen in AML—specifically, a variation of the FLT3 gene.
“This is an unprecedented collaboration of major institutions coming together to advance treatment for these cancers in the U.S.,” noted Dr. Jesus Gonzalez Lugo, assistant professor at KU Medical Center, who leads the FLT3 trial at KU Cancer Center. He believes the opportunities for screening and involvement in MyeloMATCH could be life-changing for patients.
As MyeloMATCH evolves, the initiative aims to expand the number of available substudies, with the long-term vision of creating a comprehensive pipeline where every newly diagnosed patient can receive swift diagnostic reviews and tailored treatment plans from the very start. Dr. Lin envisions a future where the MyeloMATCH framework can guide patients through their entire treatment journey, marking a transformative era in cancer care.
Stay tuned as MyeloMATCH unfolds—it could be the breakthrough we’ve all been waiting for in the fight against leukemia!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)