Groundbreaking AI Technology Allows Noninvasive Monitoring of Heart Cell Electrical Activity!
2025-01-17
Author: Arjun
Introduction
In a major leap forward for cardiac research, a collaborative team from the University of California San Diego and Stanford University has unveiled an innovative noninvasive technique that allows researchers to monitor electrical signals inside heart muscle cells without the need for invasive methods. This groundbreaking study, published in *Nature Communications*, holds immense potential for advancing medical research, drug testing, and personalized medicine.
Traditional Methods vs. New Approach
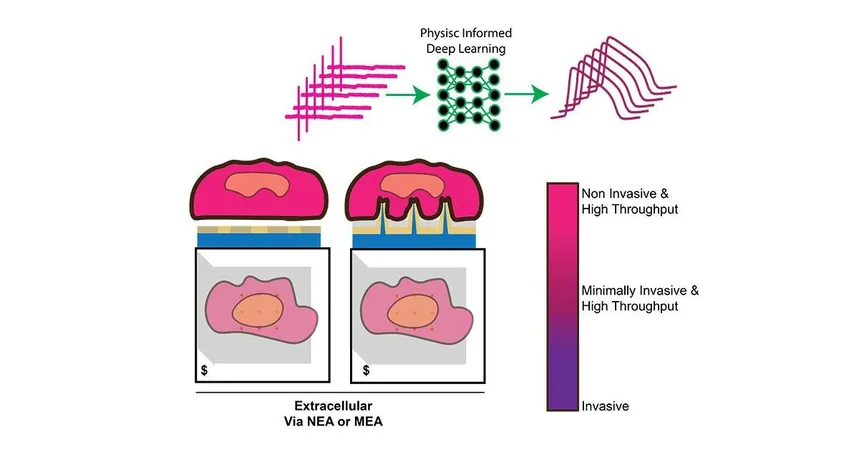
Traditionally, capturing these vital electrical signals within heart muscle cells required puncturing the cells with delicate electrodes—a process that could damage the cells and complicate large-scale testing. With the new AI-driven approach, scientists can now "listen" to the electrical communication within cells without ever touching them.
Extracellular and Intracellular Signals
The researchers focused on understanding the relationship between the electrical signals recorded on the cell’s surface—known as extracellular signals—and the deeper, intracellular signals that provide insights into the heart’s functionality and its reactions to different drugs. "We discovered that extracellular signals hold the information we need to unlock the intracellular features that we’re interested in," explained Zeinab Jahed, one of the lead authors of the study.
Creating the Dataset
To develop this revolutionary method, the team created an intricate array of nanoscale, needle-shaped electrodes that are smaller than a human hair. Using these electrodes, the researchers gathered an extensive dataset that contains thousands of signal pairs, correlating the extracellular recordings with the corresponding intracellular signals. This critical data not only provided a window into the heart cell’s response to various pharmaceutical agents but also created an invaluable resource for future research.
AI and Deep Learning Model
By harnessing the power of artificial intelligence, the team trained a deep learning model to analyze these signal pairs and accurately predict intracellular signals from extracellular recordings. "In tests, our model was able to recreate intracellular signals with remarkable accuracy," said Keivan Rahmani, a Ph.D. student and the first author of the paper.
Implications for the Pharmaceutical Industry
The implications of this work are monumental, especially for the pharmaceutical industry. Drugs must undergo thorough cardiotoxicity testing to ensure their safety for human use—a process that is currently lengthy and can sometimes rely on animal models that do not reliably predict human outcomes. With this new method, researchers can conduct drug screenings directly on human-derived heart cells. "This approach could significantly speed up drug development timelines and reduce costs," Jahed noted.
Personalized Medicine
Moreover, because the heart cells used in the testing are derived from human stem cells, this method paves the way for personalized medicine. Researchers envision a future where medications can be tailored to individual patients by screening drugs on cells specific to them, thus predicting how they might react to specific treatments.
Future Directions
While the study concentrated on heart muscle cells, the researchers are ambitiously working to expand their techniques to other cell types, including neurons. This innovation represents not just a significant benefit for cardiology but opens a gateway for a deeper understanding of cellular activities across various tissues.
Conclusion
In conclusion, this state-of-the-art AI-driven technology may redefine the landscape of drug testing and personalized medical care, unlocking new possibilities for treatments tailored to individual needs while drastically improving the efficiency and accuracy of cardiac research. The pursuit of an enhanced understanding of human biology has never been more thrilling! Stay tuned as this exciting research continues to evolve, potentially reshaping the future of medicine as we know it.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)