Exploring Prenatal Environmental Risk Factors for Autism Spectrum Disorder: What Science Reveals
2024-09-16
Author: Arjun
Exploring Prenatal Environmental Risk Factors for Autism Spectrum Disorder: What Science Reveals
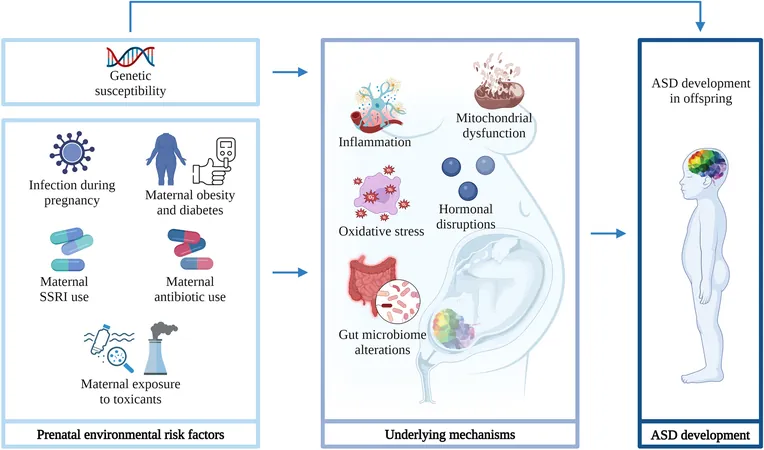
Recent research has illuminated an alarming connection between prenatal environmental factors and the risk of Autism Spectrum Disorder (ASD) in children. It has been consistently shown that maternal infections during pregnancy—specifically viral infections like rubella and cytomegalovirus—are associated with an increased risk of ASD. For example, a comprehensive study from Denmark indicated that viral infections requiring hospitalization during the first trimester, including influenza and gastroenteritis, can result in a staggering 2.8-fold increase in ASD risk. Bacterial infections during the second trimester also contributed to a 1.4-fold increase in risk, underscoring the critical timing of infections throughout gestation.
A meta-analysis encompassing 36 studies has highlighted that any maternal infection or fever elevates the chances of developing ASD by 1.3 times. Notably, fever during pregnancy has shown to double the odds of ASD, but this link seemed to diminish among those mothers who used fever-reducing medications, suggesting that such medications may alter the relationship between infection and ASD. Furthermore, genetics may play a role; a genome-wide association study from Denmark found slight genetic links between maternal infections and ASD traits in their children, albeit the genetic connection was not strong.
The Mechanisms at Play: Inflammation, Mitochondrial Dysfunction, and Gut Health
The mechanisms by which maternal infections could lead to ASD are complex. Maternal immune activation (MIA) due to infections raises pro-inflammatory cytokines, which may cross the placental barrier and affect fetal brain development. Animal studies have shown that offspring from mothers who experienced MIA exhibited behaviors akin to ASD, including social interaction deficits.
Mitochondrial function during prenatal development is another critical area of concern. Mitochondria are crucial for energy production and brain development, and disturbances caused by maternal inflammatory responses could lead to permanent neurodevelopmental challenges. Recent studies indicate this disruption could be reversible through interventions targeting mitochondrial function.
Additionally, the maternal gut microbiome may serve as a mediator between maternal infections and ASD development. Changes in the gut microbiota during pregnancy have been shown to influence fetal immune responses—impaired gut health could predispose the offspring to developmental disorders, including ASD.
The Role of Maternal Obesity and Gestational Diabetes
Maternal obesity and gestational diabetes mellitus (GDM) are also pivotal prenatal risk factors. Studies have revealed that pre-pregnancy obesity increases a child's risk of developing ASD by 1.3 to 2.0 times, while excessive weight gain during pregnancy introduces similar risks. GDM alone has been linked to a 1.5 to 1.7-fold increase in ASD likelihood. The association may stem from inflammation linked to these conditions, which can disrupt fetal neurodevelopment.
The SSRIs and Antibiotics Connection
The use of selective serotonin reuptake inhibitors (SSRIs) during pregnancy has stirred concern, with literature indicating a 1.5 to 4.5-fold increase in ASD risk depending on the trimester of exposure. Prenatal exposure to SSRIs may interfere with fetal serotonin development, an essential component of neurodevelopment.
Moreover, maternal antibiotic use during pregnancy has been implicated in raising ASD risk as well. Some studies indicate a 1.1 to 1.5-fold increase in ASD likelihood with prenatal antibiotic exposure, suggesting antibiotics may modify the effects of infections on ASD risk trajectories.
Toxic Exposures: A Hidden Danger
The impact of prenatal exposure to toxic substances, including heavy metals and air pollutants, is increasingly recognized. Substantial evidence suggests exposure to these toxicants elevates the risk of ASD by disrupting endocrine functions and increasing inflammation—factors known to influence brain development adversely.
Conclusion: A Multi-Faceted Problem
The web of factors contributing to ASD risk during pregnancy is intricate, with an interplay of infectious, metabolic, and environmental influences. It’s crucial for ongoing research to further unravel these connections, not only to inform preventive strategies but to aid in the development of personalized care approaches that can mitigate risks associated with ASD.
As we move into the next decade, the focus on how these various substrates interact will be essential in formulating interventions aimed at protecting future generations from this developmental disorder. If you’re a parent-to-be, staying informed about these risk factors could be crucial in safeguarding your child’s future health and development.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)