Exploring Healthcare-Seeking Behavior Among Patients with Non-Communicable Diseases in Rural China: A Path to Enhanced Health Outcomes
2025-01-25
Author: Arjun
Exploring Healthcare-Seeking Behavior Among Patients with Non-Communicable Diseases in Rural China: A Path to Enhanced Health Outcomes
In today's world, understanding the factors that motivate patients to seek healthcare is pivotal for designing efficient healthcare systems, particularly in rural settings. The behavior of individuals with non-communicable diseases (NCDs) in rural China underscores the need for this understanding, as it has a direct influence on healthcare utilization and the prevalence of preventable hospitalizations.
Globally, NCDs account for a staggering 41 million deaths each year, representing 74% of total mortality, with chronic diseases such as hypertension and diabetes leading the charge. Alarmingly, in China, chronic diseases accounted for 88.5% of total mortality in 2019, putting over 500 million people at risk. This crisis makes it essential to address these diseases not only through advanced medical treatments but also by encouraging patients to adopt proactive healthcare-seeking behaviors.
Understanding Healthcare-Seeking Propensity
Healthcare-seeking propensity refers to individuals' likelihood to seek medical attention based on the severity of their symptoms. Higher propensity is linked to improved health outcomes, better quality of life, and more sustainable healthcare systems. Unfortunately, in rural China, research on the healthcare-seeking tendencies of patients with chronic illnesses such as diabetes and hypertension remains scarce. Most studies focus solely on patient choices or specific illnesses, leaving a significant gap in understanding patient behaviors regarding their chronic conditions.
Applying Anderson's behavioral model of healthcare utilization, this study aims to explore the underlying factors influencing healthcare-seeking behaviors among patients suffering from hypertension or diabetes in rural China. This model identifies three primary categories affecting healthcare utilization: predisposing factors (age, gender), enabling factors (access to services, socioeconomic status), and need factors (perceived necessity of care).
Study Design and Key Findings
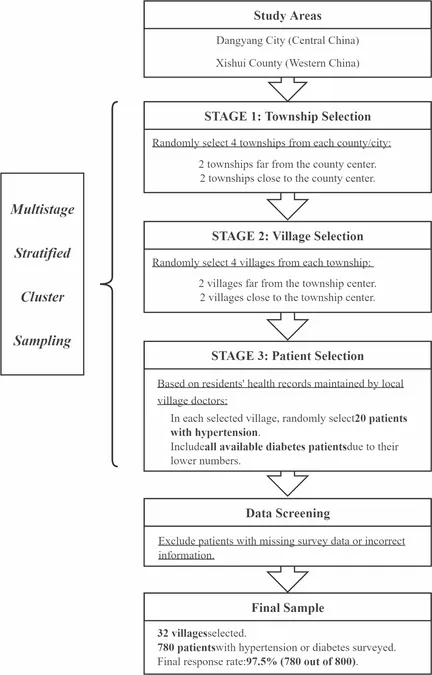
Conducted across Dangyang City and Xishui County, this cross-sectional study engaged 780 participants diagnosed with either hypertension or diabetes. By utilizing a validated questionnaire to assess healthcare-seeking propensity, it was found that various demographic factors significantly influence this behavior. Participants aged 60 and above, those with higher education levels, and individuals with above-average incomes demonstrated a greater propensity to seek care.
Accessibility to healthcare facilities also emerged as a critical factor, with shorter travel times leading to increased healthcare engagement. Conversely, individuals facing longer travel times were less likely to seek medical attention. Notably, patients with diabetes exhibited a higher inclination toward seeking healthcare compared to those with hypertension, possibly due to the more stringent self-management required for diabetes.
In terms of healthcare utilization, the analysis revealed that a higher propensity to seek treatment correlated with increased outpatient visits. Interestingly, the relationship between healthcare-seeking tendencies and preventable hospitalizations differed based on symptom severity; while major symptoms were linked to lower hospitalization rates, minor symptoms did not demonstrate a statistically significant relationship.
Regional Disparities and Implications
The findings also highlighted regional disparities, with patients in central rural areas showing higher healthcare-seeking scores than their western counterparts. These differences can be attributed to demographic and economic factors, including population age, education, and healthcare accessibility.
Navigating Future Challenges
Despite the valuable insights garnered from this study, limitations exist. The lack of granular data on the specific types and combinations of chronic diseases among participants impedes a deeper understanding of their impact on healthcare-seeking behaviors. Future research should aim to collect comprehensive clinical data to explore these nuances further.
Taking action based on these findings could enhance healthcare delivery in rural China. Improved accessibility to facilities, tailored education initiatives for chronic disease management, and streamlined relationships with healthcare providers can lead to better health outcomes and reduced healthcare costs.
In conclusion, enhancing healthcare-seeking behaviors among patients with NCDs can create a more efficient healthcare system, mitigate preventable hospitalizations, and improve overall community health in rural China. With a concerted effort towards understanding and addressing the drivers of these behaviors, the healthcare landscape in rural areas can be transformed for the better.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)