Escalating Drug-Resistant Infections in Viral Lung Patients: A Bitter Wake-Up Call
2025-08-25
Author: Siti
Respiratory tract infections (RTIs) are among the leading causes of illness and death worldwide, with viruses being the primary triggers for these acute conditions. In recent times, the emergence of viral respiratory tract infections (VRTIs), particularly concerning strains of influenza and COVID-19, has erupted into significant public health crises, spreading rapidly across the globe.
The World Health Organization reports staggering statistics: seasonal flu alone accounts for between 290,000 to 650,000 deaths yearly. Meanwhile, the COVID-19 pandemic continues to exert tremendous pressure on health care systems, with over 776 million cases and over 7 million deaths reported as of late October 2024. This growing number of hospitalizations has raised alarms about the rising rates of infections caused by drug-resistant pathogens (DRPs) among patients suffering from VRTIs.
In particular, drug-resistant infections are frequently complicating cases of viral pneumonia, posing a severe threat to critically ill patients. This surge in resistance can be attributed to various risk factors, including compromised immune systems in severely ill patients and the increased use of high-dose glucocorticoids in treatment.
Awareness is growing surrounding the inappropriate use of broad-spectrum antibiotics among COVID-19 and flu patients, raising the stakes in managing these infections. Addressing these challenges requires a robust analysis of the antibiogram profiles of drug-resistant bacterial isolates from VRTI patients. An understanding of the risk factors contributing to nosocomial DRPs is essential for devising effective treatment strategies.
Recently, artificial intelligence (AI) has emerged as a promising tool for predicting disease outcomes. Machine learning (ML) algorithms, in particular, have shown prowess in recognizing complex patterns, leading researchers to advocate for their integration into clinical practice. However, there’s a noticeable gap in existing studies regarding the risk factors associated with DRP infections, highlighting the need for more comprehensive research.
Study Overview and Objectives
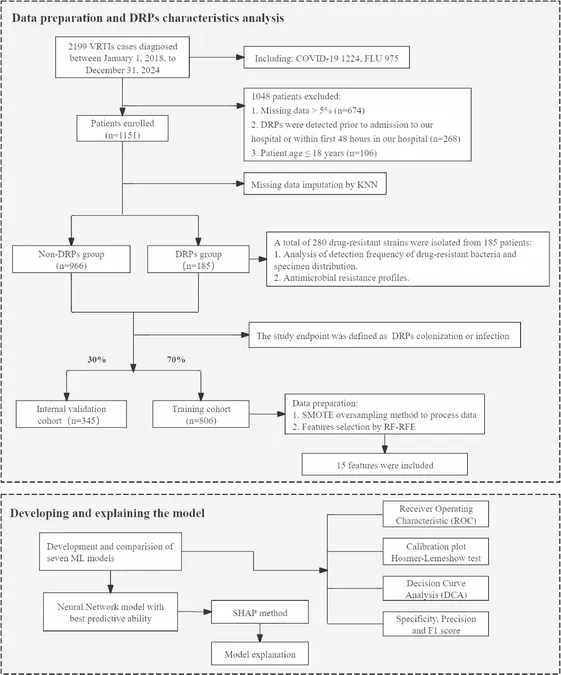
This study aims to conduct a thorough antibiogram analysis of drug-resistant strains isolated from patients with VRTIs complicated by DRPs. In addition, an interpretable ML model will be developed to identify key risk factors associated with hospital-acquired DRPs. Data was retrospectively gathered from over 2,000 patients at Beijing Ditan Hospital between 2018 and 2024, with strict inclusion and exclusion criteria ensuring the reliability of the findings.
Patient Profile and Research Methodology
In and out of the rigorous screening processes, 1,151 eligible cases were identified for analysis. The study focused on various variables, including demographic data and clinical parameters gathered from electronic medical records (EMRs). Comprehensive data collection aimed to expose crucial insights into antibiotic resistance patterns and specific risk factors for hospital-acquired DRP infections.
Key Findings on Drug-Resistant Strains
The analysis revealed significant insights into distribution and resistance among bacterial pathogens. A staggering 75.73% of isolates were Gram-negative bacteria, with strains like Pseudomonas aeruginosa and Klebsiella pneumoniae showing alarmingly high resistance rates to multiple antibiotics. This study underscores the urgent need for continued vigilance against the escalating threat of carbapenem-resistant bacteria.
Machine Learning Model for Predicting Infections
The neural network model developed in this study displayed outstanding accuracy in identifying the risk factors linked to hospital-acquired DRPs. Key variables like length of stay (LOS), biochemical markers, and age were critical in predicting the likelihood of developing these infections, providing a potential decision-making tool for clinicians.
The findings emphasize how factors such as prolonged hospital stays and invasive procedures correlate strongly with increased risk. Moreover, a novel association between low levels of cholinesterase and DRP infections was uncovered, suggesting deeper paths to explore for therapeutic options.
Conclusion and Implications for Future Research
This study sets a foundational framework for understanding the dynamics of drug-resistant infections in patients with viral respiratory conditions. As drug resistance poses a growing threat in clinical settings, the integration of machine learning tools into treatment protocols could significantly bolster clinical outcomes. Moving forward, it is crucial for researchers to embrace multicenter collaborations, expanding the understanding of antibiotic resistance and refining predictive models for better patient management.
The research highlights an urgent call to action for health care professionals to reevaluate antibiotic use, promote careful surveillance of resistance trends, and fortify strategies against these formidable drug-resistant pathogens.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)