Enhancing Geriatric Rehabilitation: The Crucial Role of Interprofessional Collaboration in Multidisciplinary Team Meetings
2025-03-29
Author: Mei
The Structure of MDTMs and the Need for IPC
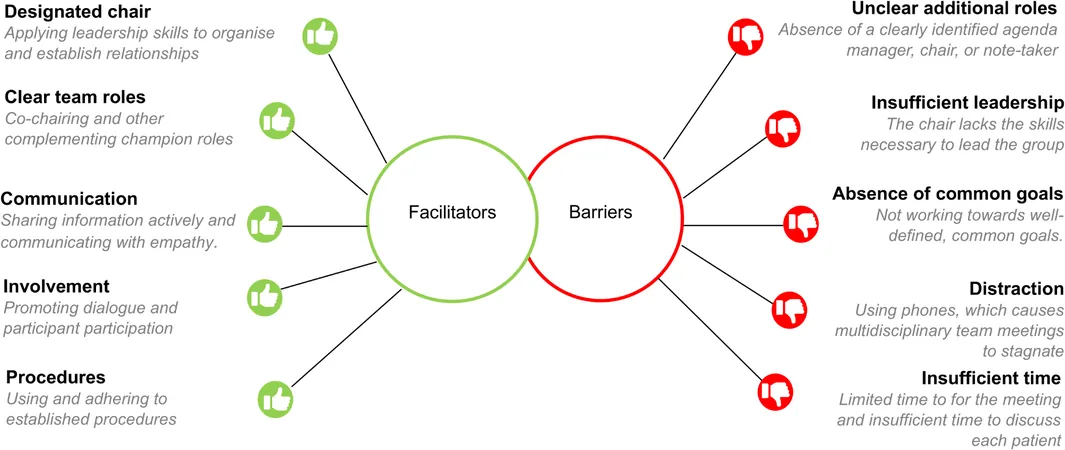
Recent observational studies have indicated that effective IPC during MDTMs can significantly enhance the rehabilitation process. Successful MDTMs necessitate structured communication, coordinated procedures, and active participation from all stakeholders, including patients and caregivers. Research highlights that when individuals from various professions actively collaborate and share information, the outcomes for patients improve markedly.
Key Findings from the Observational Study
The study was conducted across seven MDTMs within four geriatric rehabilitation facilities in the Netherlands, with data collection occurring from May to December 2022. Key findings from the observational analysis included: 1. **Team Performance**: Clarity in team roles and responsibilities emerged as a significant factor in facilitating effective IPC. The presence of designated roles, particularly that of a chairperson, ensured that meetings were well-organized and focused on shared goals. 2. **Organizational Conditions**: Adequate time for discussion and a structured agenda were crucial for thorough patient evaluations. However, time constraints often pressured teams to rush through discussions, which could compromise the quality of care. 3. **Information Sharing**: Effective communication among team members was vital. When team members actively shared and discussed information regarding patients' conditions, it led to better understanding and coordination of care. 4. **Use of Patient Outcome Measures**: Although recommended, the utilization of standardized patient outcome measures was found to be limited. Incorporating these measures could aid in articulating patient needs and fostering a common language among healthcare providers.
The Benefits of Enhanced IPC
Participants in MDTMs expressed high levels of satisfaction with the collaborative efforts observed, rating their experiences favorably. However, comments also revealed a desire for improvement in transdisciplinary focus and involvement of all relevant parties, including patients and caregivers. The need for a shift from merely interdisciplinary approaches to true collaborative practices was noted. Furthermore, engaging patients and caregivers significantly enhances the rehabilitation experience, fostering shared decision-making and personalizing care plans. Encouraging their participation in MDTMs is essential for realizing the goals of person-centered rehabilitation.
Moving Forward: Recommendations for Future Research and Practice
To enhance IPC in geriatric rehabilitation, future studies should focus on the following areas: - **Patient and Caregiver Involvement**: Research should explore innovative ways to integrate patients and caregivers into MDTMs, ensuring their voices are heard and their perspectives inform care strategies. - **Methodical Use of Outcome Measures**: Investigating barriers to the use of patient outcome measures will illuminate pathways for their more consistent application, enhancing the quality of evaluations during MDTMs. - **Training and Support for Team Leaders**: Providing leadership training and resources for chairpersons in MDTMs can foster better facilitation of meetings, ensuring that they are inclusive and structured effectively.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)