Critical Case: 18-Day-Old Baby's Battle with Mysterious Breathing Issues
2025-05-07
Author: Sarah
The Start of a Distressing Journey
An 18-day-old baby girl was rushed to the Emergency Department, battling alarming symptoms: episodes of apnea, cyanosis, and inadequate feeding. Her mother detailed troubling signs including lip cyanosis, pale skin, and suspected breathing pauses. Since her birth, the infant exhibited retractions, which her primary care provider had reassured were typical periodic breathing. However, after her discharge from the nursery, she also developed nasal flaring and grunting, further heightening maternal concerns. Periods of rapid breathing, clocking in the 60s or 70s per minute, were also noted.
Initial Assessment and Alarming Vitals
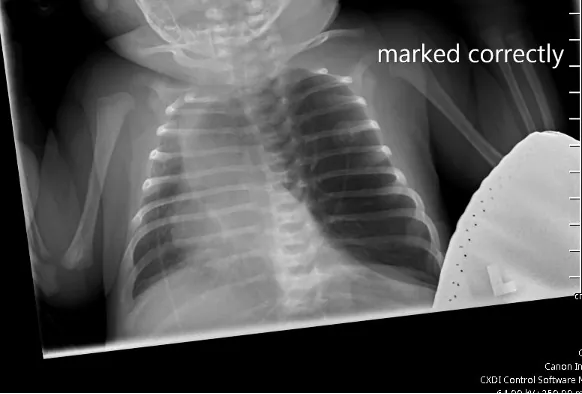
Upon arrival at the ED, the infant exhibited hypoxemia and tachypnea, with oxygen saturation levels fluctuating wildly between 65% and 100% while on room air. The medical team quickly ordered a chest X-ray to investigate further.
A Distressing Physical Examination
During a thorough physical examination, it was evident that the baby was in significant respiratory distress. With an oxygen saturation level of 96% on high-flow nasal cannula and severely decreased airflow bilaterally, concerns began to mount. Further tests, including a complete blood count and metabolic panel, revealed normal results. However, a venous blood gas analysis raised alarm with values of 7.24/74/51/35.
Unveiling the Mystery: Tension Pneumothorax or Something Else?
While on the pediatrics floor, an X-ray raised the possibility of a tension pneumothorax, prompting a swift transfer to the Pediatric Intensive Care Unit (PICU). An urgent needle decompression was performed, but no improvement in vitals was observed—no rush of air signified the suspected condition. To clarify the situation, a CT scan with IV contrast was conducted.
A Life-Changing Discovery
The CT scan confirmed a diagnosis of left upper lobe congenital emphysema. The medical team proceeded with surgical resection of the affected lung lobe, after which the baby's respiratory situation significantly improved, demonstrating the critical need for prompt intervention.
Understanding Congenital Lobar Emphysema
Congenital lobar emphysema (CLE), a rare yet severe pulmonary disorder primarily impacting neonates, was the underlying cause in this case. Characterized by hyperinflation of lung lobes—most often the left upper lobe—this condition emerges from defects in airway cartilage causing airflow obstructions. Such obstructions lead to air trapping and can compress surrounding lung tissue, resulting in respiratory distress, as witnessed here.
Diagnosis and Management: A Complex Path
Diagnosing CLE can be tricky, especially as it closely resembles other conditions like tension pneumothorax. Imaging via chest X-rays and CT scans are typically needed for accurate confirmation. In this case, the initial red flags from the X-ray set the stage for the eventual diagnosis confirmed by CT findings of hyperinflation and atelectasis in the left lobe.
The Road to Recovery
While treatment for CLE often starts with supportive care and may necessitate mechanical ventilation, definitive treatment usually involves surgical removal of the affected lobe (lobectomy). This is particularly vital when hyperinflation leads to critical respiratory distress. Following the removal of the problematic left upper lobe, the baby’s condition improved dramatically.
The Takeaway: Timely Intervention is Key
This case underscores the absolute necessity for early recognition and intervention in neonates facing severe respiratory distress. Prompt surgical techniques can not only be lifesaving but also prevent enduring complications related to untreated congenital lobar emphysema.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)