
COVID-19 Linked to Alzheimer’s-Related Changes in the Retina: A New Study's Groundbreaking Findings
2025-07-14
Author: Sarah
A striking new study from Yale University suggests that COVID-19 may not only result in brain fog but could also play a role in accelerating Alzheimer’s disease by promoting dangerous amyloid beta buildup in the retina.
Breakthrough Research Linking COVID-19 and Alzheimer’s Symptoms
Research has long indicated that amyloid beta peptides—small chains of amino acids—contribute to the formation of plaques that are a hallmark of Alzheimer’s disease. These plaques may actually serve as a protective measure against infections like bacteria and viruses. Importantly, the integrity of the blood-brain barrier often diminishes in Alzheimer’s patients, making this accumulation a potential signal of pathogen infiltration into the brain.
What the Yale Study Revealed
In this groundbreaking study, published in *Science Advances*, Yale researchers delved into the potential connection between SARS-CoV-2, the virus responsible for COVID-19, and the onset of Alzheimer’s-like amyloid beta buildup. Senior author Dr. Brian Hafler, an associate professor at Yale School of Medicine, highlighted the increasing evidence linking COVID-19 with cognitive difficulties.
Exploring the Retina: A Window into the Brain
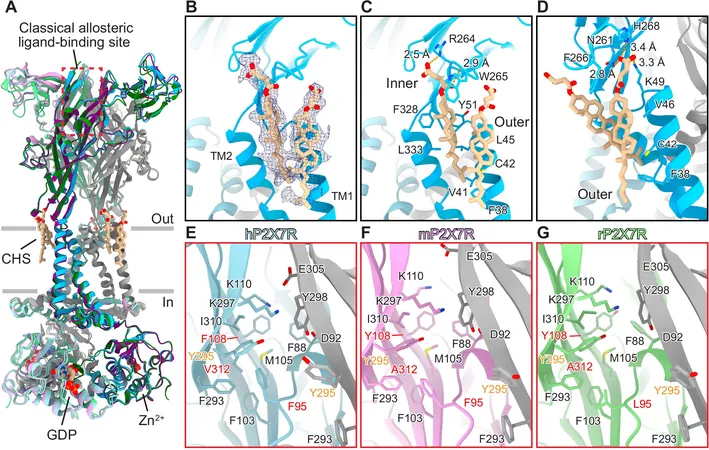
The researchers utilized human retinal organoids—miniature, lab-grown versions of retinas—to mimic the conditions of Alzheimer’s disease. These organoids were designed to replicate genetic mutations that lead to increased amyloid beta production, providing valuable insights into the disease's progression.
Remarkably, the study confirmed that amyloid beta accumulation, commonly observed in Alzheimer’s patients, was also present in the retinal tissue examined. According to Dr. Hafler, the retina offers a unique, non-invasive perspective into the brain's activity.
How SARS-CoV-2 Enters Retinal Cells
The researchers discovered that the SARS-CoV-2 virus could enter retinal cells. By analyzing the presence of proteins known to assist viral entry—specifically NRP1 and ACE2—the team found that cells from individuals who had contracted COVID-19 exhibited these entry mechanisms. When they exposed their retinal organoids to the SARS-CoV-2 spike protein, a significant increase in amyloid beta levels was observed.
Impact on Human Retinal Tissues
Additionally, human retinal samples from COVID-19 patients with no prior history of dementia displayed amyloid beta accumulation levels mirroring those seen in individuals with Alzheimer’s. Interestingly, this accumulation was reversible with an NRP1 inhibitor treatment—indicating a potential therapeutic avenue.
Opening Doors for Future Research
This study illuminates new paths for combating COVID-related cognitive decline. Dr. Hafler emphasized how these findings not only reinforce the connection between infectious agents and Alzheimer’s but also propose that amyloid beta could play a role in the brain's immune response to viral invaders. Further research is essential to fully understand these dynamics.
The Road Ahead: Research Goals
With lingering neurological symptoms from COVID-19 such as brain fog, Hafler's team is conducting clinical trials to explore whether SARS-CoV-2 infection heightens the risk of Alzheimer’s disease over time and how early intervention might mitigate this risk. Their ultimate aim? To prevent the long-term neurological effects of COVID-19 and investigate NRP1 inhibitors as a potential treatment to thwart viral-related amyloid pathology.
This important research was supported by National Institutes of Health grants and other foundations, marking a pivotal step in understanding the intersection of viral infections and neurodegenerative diseases.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)