COVID-19 and Pregnancy: New Insights into Risks, Comorbidities, and Health Outcomes
2024-11-14
Author: Jia
Pregnant Women at Risk
Pregnant women are considered a high-risk group for severe illness from COVID-19, especially when they have pre-existing comorbidities. Studies indicate that underlying health issues—ranging from diabetes and chronic lung diseases to mental health disorders—can significantly elevate the risks associated with a COVID-19 infection. This is corroborated by data showing that pregnant women with COVID-19 experience higher rates of adverse outcomes, including hospitalization and even maternal mortality.
For instance, a disturbing report from Brazil highlighted a 12.7% mortality rate for pregnant women with COVID-19 during both pregnancy and the postpartum period. Similarly, data from the UK revealed a correlation between moderate to severe COVID-19 and increased perinatal complications, particularly among unvaccinated women during the dominant delta variant phase.
The Complex Role of Immunity
Interestingly, the immunosuppressed state of pregnancy has been a subject of debate. Some studies suggest that this immune modulation may offer a paradoxical protective effect against severe COVID-19 symptoms, potentially reducing the risk of cytokine storms which can be fatal. However, the relationship remains intricate; pregnant women may still face heightened risks if they have other causes of immunosuppression.
Research continues to point out the need for health systems to broaden their understanding of the factors influencing the health of pregnant women during the pandemic, specifically focusing on comorbidities like chronic obstructive pulmonary disease (COPD), chronic renal disease, and mental health conditions.
Insights from Data Analysis
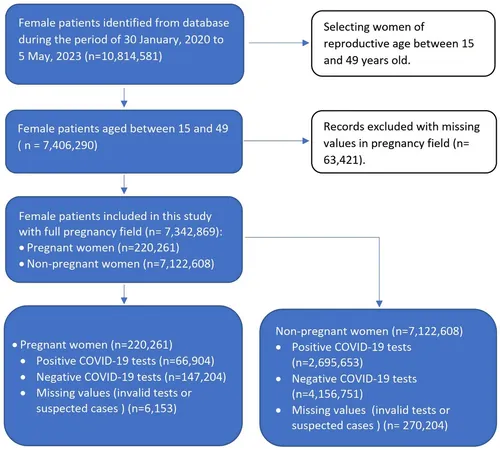
In a massive cohort analysis including over 10 million women, the results revealed several alarming trends. Approximately 30% of the 220,261 pregnant women studied were confirmed cases of COVID-19, with these women facing greater health challenges compared to non-pregnant women. Pregnant women demonstrated a higher likelihood of pneumonia, hospital admissions, and requirements for intensive care.
This was starkly illustrated with pregnant women facing a fourfold increase in the likelihood of hospitalization and intubation compared to non-pregnant women. Furthermore, certain comorbidities, including diabetes and renal disease, significantly elevated COVID-19-related hospitalizations for both groups.
The Death Rate Dilemma
Frighteningly, the mortality rate in pregnant women infected with COVID-19 is approximately 6.5 times higher than those without the infection, indicating a critical area for intervention. Factors such as age, diabetes, and intubation treatments have been identified as considerable risk enhancers for mortality among pregnant women.
Conversely, the overall findings suggest that pregnant women had a lower mortality rate compared to non-pregnant women, leading to ongoing debates about COVID-19's impact on pregnant women versus the general population's health risks.
Guidelines for Future Research
Given the disparities revealed by this study, particularly concerning renal disease and immunosuppression as prominent risk factors, there's a need for targeted clinical guidelines. Recommendations for managing COVID-19 in pregnant women should prioritize early intervention, tailored healthcare strategies for those with comorbidities, and special attention for higher-risk groups.
Furthermore, healthcare systems must harness this data to develop robust risk assessment mechanisms and management protocols, thus ensuring better maternal and fetal outcomes during health crises.
In conclusion, while pregnant women face heightened risks during the COVID-19 pandemic, understanding and addressing the complexities of their health outcomes is vital. Continuous research, informed clinical practices, and adequate health service planning are critical in combating the repercussions of COVID-19, especially as new variants and challenges emerge. The health of mothers and their babies hangs in the balance, demanding urgent further investigation and effective intervention strategies.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)