Could SARS-CoV-2 Be Unlocking Secrets to Alzheimer's? New Study Reveals Shocking Connections!
2025-07-14
Author: Siti
A groundbreaking study from Yale has uncovered a compelling link between COVID-19 and the alarming buildup of amyloid beta peptides—one of the key culprits behind Alzheimer's disease. As we navigate the aftermath of the pandemic, this research shines a light on the neurological challenges some experience post-infection, often dubbed 'brain fog'.
Alzheimer's disease is notorious for its amyloid beta plaques, which accumulate around brain cells. While traditionally thought to guard the brain against infections, researchers now believe that a compromised blood-brain barrier in Alzheimer’s patients may allow pathogens to penetrate the brain, triggering these dangerous plaques.
The COVID Connection: Unraveling the Mystery of Brain Fog
The Yale team's study, published in 'Science Advances', probes whether SARS-CoV-2, the virus responsible for COVID-19, triggers this amyloid beta accumulation, leading to cognitive impairments. Senior author Dr. Brian Hafler states, "There is increasing evidence suggesting a connection between COVID-19 and brain fog, a symptom that closely mirrors what Alzheimer's patients experience."
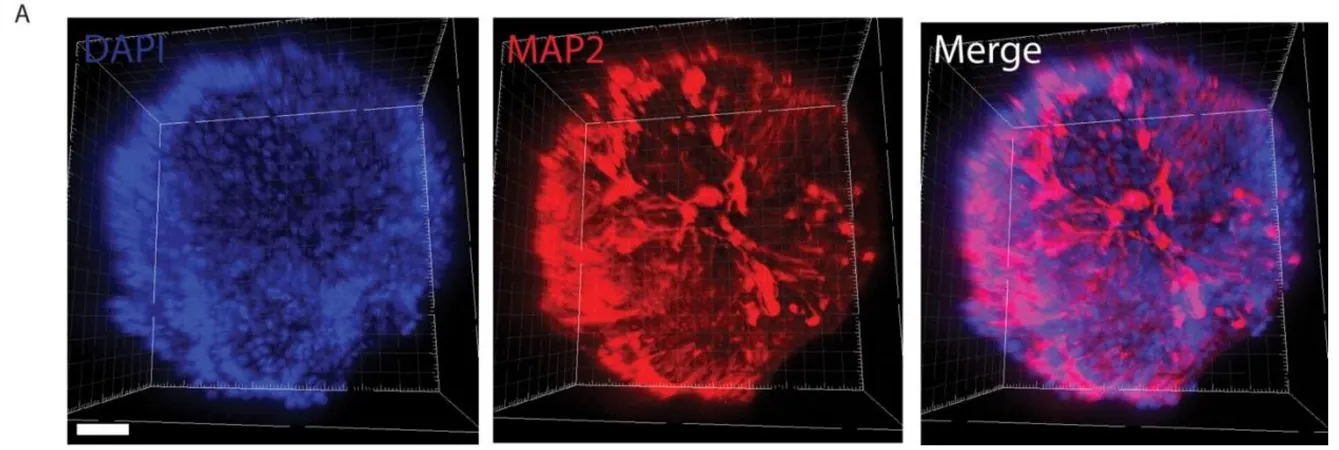
Inside the Lab: Using Retinal Organoids to Make Breakthroughs
To investigate this, Hafler's team turned to retinal organoids—miniature, lab-grown human retinal tissues molded from stem cells. These organoids exhibited characteristics of Alzheimer’s, including excessive amyloid beta production. Hafler emphasizes the advantage of using human retinal organoids, saying, "This model avoids the complications of animal-based studies, allowing us to focus on human cellular responses.”
Remarkably, the researchers confirmed that amyloid beta, prevalent in Alzheimer’s, was also detected in the retina, which serves as a non-invasive window into the central nervous system.
Virus on the Loose: How SARS-CoV-2 Enters the Retina
The team discovered that SARS-CoV-2 can infiltrate retinal cells. By analyzing protein production within different retinal cell types, they identified critical proteins, NRP1 and ACE2, known to facilitate the virus's entry. In retinal tissues from COVID-19 patients, NRP1 presence in neurons and glial cells suggested a vulnerability within the eye to viral invasion.
Echoes of Alzheimer's: Increased Amyloid Beta Accumulation Found
When exposed to the SARS-CoV-2 spike protein, the retinal organoids showed a significant rise in amyloid beta levels. They also found that human retinal tissues from COVID-19 patients—who had no history of dementia—revealed amyloid beta levels alarmingly similar to those seen in Alzheimer's patients.
A Possible Game-Changer in Treatment?
Encouragingly, the research indicated that administering an NRP1 inhibitor reversed this amyloid beta buildup in retinal samples exposed to the spike protein. Hafler notes that targeting NRP1 as a molecular lever could lead to transformative therapies for neurological complications following COVID-19.
Opening New Doors for Future Research
This study reinforces the notion that infections could play a role in Alzheimer's progression. Hafler suggests that amyloid beta might be a part of the brain’s defense mechanism against viral incursions. "We need to explore if similar allergic reactions occur with other viral infections," he adds.
With ongoing clinical studies at Yale investigating the long-term risks of Alzheimer’s after SARS-CoV-2 infection, the quest continues. Hafler's ultimate goal is to mitigate the neurological aftermath of COVID-19 by developing therapies targeting virus-host interactions and preventing amyloid-related pathology.
As more insights come to light, the hope is that we could unlock not just treatments for brain fog but also for Alzheimer’s itself!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)