Cervical Cancer Survivors Face Increased Risk of Anal Cancer—Here's What You Need to Know!
2025-09-12
Author: Mei
A Shocking Discovery: The Link Between Cervical and Anal Cancer
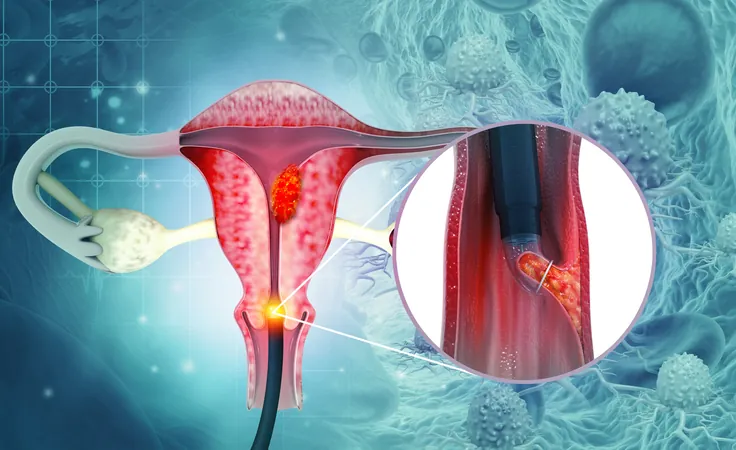
New research from the Hollings Cancer Center at the Medical University of South Carolina reveals a startling fact: women who have battled cervical cancer are nearly twice as likely to develop anal cancer compared to those without such a history. This connection is attributed to the human papillomavirus (HPV), the notorious culprit behind both types of cancer.
Cervical Cancer: A Global Challenge
Cervical cancer originates from HPV infections, primarily spread through sexual contact, disrupting the natural cellular structure in the cervix. While the survival rate for early-detected cervical cancer can soar beyond 90%, the reality is more alarming: in 2022, there were over 660,000 new cervical cancer cases worldwide, leading to approximately 350,000 fatalities. Despite advancements in HPV vaccination and screening in wealthier nations, lower-income regions are still grappling with high incidence rates.
A Call for Awareness—Understanding the Risks
However, there's a troubling lack of follow-up protocols for cervical cancer survivors, leaving many unaware of their elevated risks for related cancers. To shed light on this, the researchers sought to determine whether a history of cervical cancer significantly elevates the odds of developing anal cancer.
Co-author Ashish Deshmukh, PhD, emphasizes, "We’ve known for a long time that both cancers are linked through HPV, but the extent of this risk connection hasn’t been well-explored."
The Groundbreaking Study—What They Found
Their pivotal study, published in the journal JAMA Network Open, analyzed data from the National Cancer Institute, encompassing 85,524 women diagnosed with cervical cancer from 1975 to 2021. Alarmingly, 64 of these women subsequently developed anal cancer within 20 years.
The statistics are staggering. Younger women (under 45) had an anal cancer incidence rate of 2.4 per 100,000, while women aged 45 to 54 faced 4.6 per 100,000. This soared to 10 for those aged 55-64 and peaked at 17.6 for women aged 65-74—a clear indication that risks climb with age.
Why the Delay? Understanding the HPV Virus
The delay in anal cancer diagnosis can stretch 15 to 20 years post-cervical cancer due to the insidious nature of HPV. The virus can linger, oftentimes undetected, expanding its reach within the body over the years. As Deshmukh explains, the subtleness of symptoms makes timely detection challenging.
Essential Screening Recommendations for Survivors
Currently, routine anal cancer screenings are reserved for high-risk individuals such as those living with HIV or those who've had organ transplants. However, the new findings suggest that survivors of cervical cancer should also be included in these high-risk categories.
"Screening everyone isn't feasible, but targeting those at highest risk ensures we provide critical care where it’s desperately needed," states Deshmukh.
Future Directions—Researching Further to Protect Survivors
The research team is now focused on pinpointing the highest-risk patients, assessing the pros and cons of screening, determining optimal starting ages, and establishing effective screening intervals. Their ultimate aim? To ensure long-term cancer survivors don't just survive one battle but are empowered to prevent another.
As Damgacioglu puts it, "These women have already fought against cancer—we are committed to helping them defend their health against the possibility of a second fight."


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)