Cefepime vs. Carbapenems: Which is More Effective for Complicated Urinary Tract Infections?
2025-03-31
Author: Rajesh
Introduction
In the world of medicine, complicated urinary tract infections (cUTIs) pose a significant challenge, especially in patients who are critically ill. This type of infection is not only a leading cause of sepsis—accounting for 20-40% of mortality in these patients—but also a condition that increasingly affects immunocompromised individuals or those with abnormalities that hinder effective urine flow. With an aging population, widespread use of immunosuppressants, and invasive procedures, the incidence of cUTIs is on the rise worldwide, which brings a considerable healthcare burden associated with the growing bacterial resistance to treatment.
Challenges in Treatment
Among the culprits behind cUTIs, Enterobacterales—such as Enterobacter spp., Serratia marcescens, and others—are notorious for harboring chromosomally encoded AmpC β-lactamase genes, confounding the treatment efforts. As traditional treatments like carbapenems become less effective due to rising resistance, the search for alternative therapies is critical. One potential candidate is cefepime, a fourth-generation cephalosporin noted for being a weak inducer of AmpC production.
Recent Guidelines
Recent guidelines from the Infectious Diseases Society of America suggest cefepime as a viable alternative to carbapenems in cases involving organisms likely to produce AmpC, provided their minimum inhibitory concentration (MIC) stays at 2 µg/mL or lower. However, confusion remains concerning cefepime’s effectiveness against co-producing extended-spectrum beta-lactamases (ESBLs), with various studies indicating alarmingly high rates of co-production across countries.
Study Overview
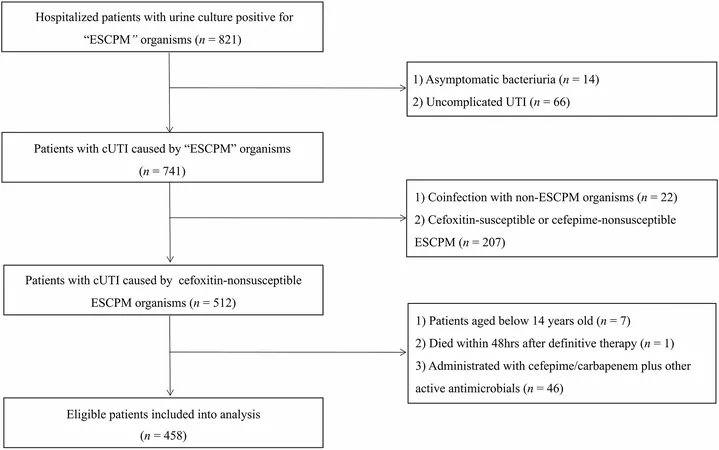
The current multicenter study discussed focused on comparing cefepime and carbapenems in treating cUTIs caused by cefoxitin-non-susceptible Enterobacterales that are cefepime-susceptible. Data was collected from four teaching hospitals in China from January 2010 to December 2022. The study included 458 patients who fit the criteria, aiming to assess treatment failures within 14 and 28 days, with tailored therapies provided based on drug susceptibility testing.
Patient Population and Findings
The analyzed cohort consisted mainly of older adults—median age 67—with a range of comorbidities, including cardiovascular conditions, chronic kidney disease, and diabetes. Treatments varied, with a notable number receiving either cefepime or carbapenems, and the outcomes were telling:
- **14-Day Treatment Failure Rate**: Approximately 18.1%
- **28-Day Treatment Failure Rate**: Approximately 15.7%
- **Clinical Response Rate**: Improved responses were noted in those treated with cefepime compared to carbapenems.
Interestingly, the study discovered that patients treated with cefepime tended to have fewer chronic illnesses and experienced reduced rates of secondary bacteremia and septic shock, suggesting that cefepime could be associated with more favorable outcomes in certain patient populations.
Predictors of Treatment Failure
The multivariate analyses highlighted several predictors for treatment failure after 28 days: the patient's age, the efficacy of empirical therapy, and immunocompromised status played pivotal roles. Strikingly, the research illustrated that while cefepime may provide adequate coverage for certain strains, carbapenems demonstrated superior efficacy against some strains of AmpC-producing bacteria.
Key Takeaways and Implications
This study emphasizes the necessity for personalized treatment approaches, taking into account the unique risk factors and microbiological profiles of patients with cUTIs. As bacterial resistance increasingly complicates the treatment landscape, understanding the nuances between antibiotic classes becomes crucial—not just for immediate patient care, but also for public health strategies against multidrug-resistant organisms.
The findings support cefepime as a potentially effective option for specific patient groups, though the greater potency of carbapenems against certain bacterial strains suggests they should remain a primary option in more severe cases. Ultimately, the battle against cUTIs is far from over, and ongoing research will be vital in adapting our clinical approaches to these evolving medicinal challenges.
Conclusion
In conclusion, while cefepime shows promise, healthcare providers must remain vigilant about resistance trends and adjust treatment protocols accordingly. This strengthens the idea that tailored approaches, considering both clinical and microbiological characteristics, are key to improving outcomes in patients with complicated urinary tract infections.
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)