CDC Unveils New Resources for Managing Post-Lyme Disease Symptoms: What Patients and Doctors Need to Know!
2024-09-23
CDC Unveils New Resources for Managing Post-Lyme Disease Symptoms
In a recent CDC webinar aimed at clinicians, experts launched a crucial new toolkit designed to aid physicians in addressing the challenges faced by patients suffering from prolonged symptoms following Lyme disease treatment. This innovative resource comes in response to increased awareness of the complexities surrounding Lyme disease and its aftereffects.
"Lyme disease is not just a medical issue, but a social phenomenon," emphasized Dr. Grace Marx, MD, MPH, from the CDC’s division of vector-borne diseases. She highlighted the challenges that ensue from a mix of patient desperation for answers, physician frustration, and rampant medical misinformation. "It’s essential for physicians to approach these clinical encounters with a solid understanding grounded in science," she added.
Understanding Lyme Disease
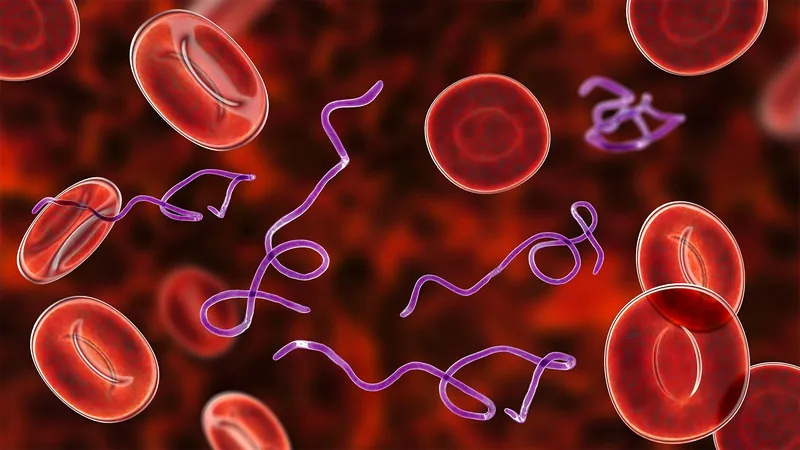
Lyme disease, caused by the bacterium Borrelia burgdorferi transmitted via the Ixodes blacklegged tick, requires prompt diagnosis and treatment. Early detection is vital to prevent the disease from progressing. Treatment typically involves a course of antibiotics lasting from 10 days to 4 weeks, depending on the severity of the condition. Unfortunately, research has shown that extended courses of antibiotics provide no significant benefits over placebo for some patients.
Post-treatment Lyme disease syndrome (PTLDS), affecting 5% to 10% of those treated, can manifest as persistent fatigue, joint and muscle pain, as well as cognitive difficulties lasting six months or longer. The complexities arise, however, when patients who have not received an official Lyme diagnosis yet exhibit PTLDS-like symptoms seek validation, leading to the controversial term "chronic Lyme disease" for those lacking definitive medical evidence of infection.
Expert Insights
Dr. Erica Kaufman West, the director of infectious diseases for the American Medical Association (AMA), pointed out that many patients are grappling with symptoms that are medically unexplained, and they pursue a diagnosis fervently. It’s suggested that some of these signs could stem from other post-acute infection syndromes, such as long COVID or post-polio syndrome.
To better guide healthcare providers in managing these complex cases, the CDC and AMA, alongside Mathematica — a research firm, conducted interviews and focus groups with a diverse group of experienced physicians. Here are some key takeaways:
Key Takeaways
1. **Validation is Key**: Clinicians should actively listen and validate their patients’ symptoms. Many individuals feel dismissed by the current medical practices, which can exacerbate their conditions.
2. **Time Consumption and Exhaustion**: Both patients and physicians may feel drained during consultations, with providers carrying the burden of needing to diagnose accurately amidst a myriad of potential conditions.
3. **Symptom Overlap**: Many symptoms of PTLDS overlap with conditions such as fibromyalgia, long COVID, and chronic fatigue syndrome, making accurate diagnosis a significant challenge.
4. **Listening to Patient Narratives**: Dr. Marx emphasized the importance of thoroughly exploring each patient’s timeline of symptoms and their responses to past treatments. Comprehensive physical assessments are also fundamental.
5. **Avoiding Diagnostic Anchoring**: Physicians are encouraged not to settle prematurely on a diagnosis but to consider a wide range of potential conditions tailored to the patient’s specific symptoms and findings.
Patients feeling neglected by conventional healthcare may turn to alternative practitioners, sometimes leading to risky and unproven treatments, a phenomenon termed "medical wandering."
Resources and Toolkits for Improvement
To aid physicians in their practices, the AMA has rolled out a continuing medical education (CME) module that focuses on the complexities of Lyme disease, emphasizing the necessity of a broad differential diagnosis and an individualized care plan.
Furthermore, a clinician toolkit available on the AMA’s website features resources for both physicians and patients, including patient symptom diaries and goal trackers aimed at documenting personal health journeys and focusing on specific, measureable outcomes. For instance, what could be a significant achievement for one patient might differ vastly from another's goals.
Ultimately, the objective of this new toolkit is not solely to attain a diagnosis but to enhance the quality of life for patients enduring chronic pain or suffering from other lingering effects. Dr. Kaufman West stated, "The goal is to improve these patients' lives, focusing on reducing pain days and enhancing overall quality of life."
With these advancements, the CDC and AMA aim to better equip healthcare providers to meet the evolving needs of Lyme disease patients, fostering a supportive environment that prioritizes comprehensive care and understanding.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)