Breakthrough Study Reveals Mixed Outcomes in Post-Stroke Fever Management
2024-09-25
Author: Sarah
Introduction
In a groundbreaking study aimed at improving the recovery of stroke patients, researchers have unveiled surprising results regarding fever prevention in intensive care units (ICUs). The INTREPID randomized trial showcased a dedicated temperature management device that effectively reduced fever occurrences in stroke patients. However, the study’s findings raise important questions about the real-world benefits of this intervention.
Trial Overview
Conducted internationally among neurocritical care patients with vascular brain injuries, the trial found that using the fever prevention device led to a significant decrease in daily mean fever burden compared to standard care. The average temperature hours recorded were 0.37 °C-hour for those receiving the temperature management treatment versus 0.73 °C-hour for the control group, clearly demonstrating the device’s utility (P<0.001). Additionally, the treatment group experienced far fewer hours of fever—9.0 hours versus 21.6 hours for the control group.
Functional Outcomes
Despite these optimistic numbers, the study led by Dr. David Greer from Boston University School of Medicine revealed a troubling paradox: there were no improved functional outcomes for patients after three months. Both groups exhibited identical median scores on the modified Rankin Scale (mRS), commonly used to measure rehabilitation success after a stroke, scoring a 4.0. The likelihood of achieving a good outcome (mRS scores of 0-3) remained statistically unchanged (39.2% in the treatment group vs. 42.8% in the control group).
Possible Explanations
The investigators provided several possibilities for these unexpected results. They noted that while the fever management technique was successful, some patients (about 8%) could not endure the therapy due to side effects such as shivering and discomfort. Furthermore, the most significant temperature differences between the groups were observed only during the first five days of ICU treatment, suggesting that prolonged care might not be necessary for some patients. It was also mentioned that one in four patients in the control group never experienced a fever, implying that the need for fever prevention might not be ubiquitous.
Study Conclusion
The trial's recruitment halted prematurely after enrolling 686 participants, well below the targeted 1,176 patients, due to an assessment of futility—the expectation that the treatment would not significantly improve outcomes. This early stoppage only intensifies the debate surrounding the effectiveness of such a targeted intervention in varying stroke populations.
Expert Commentary
Experts Teresa May from Maine Medical Center and Lori Shutter from the University of Pittsburgh School of Medicine commented on the implications of the study, suggesting that the lack of homogeneous responses in stroke patients necessitates a more tailored approach in future research. They emphasized the importance of identifying specific patient demographics that would potentially benefit from fever prevention strategies.
Trial Details
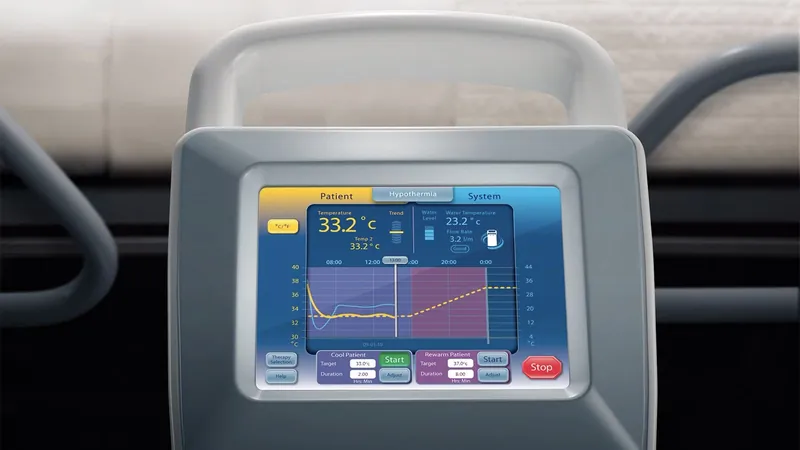
Conducted between 2017 and 2021 across seven countries, the INTREPID trial focused on patients suffering severe strokes, including ischemic strokes and various forms of hemorrhagic strokes. The fever management technique employed the Arctic Sun, an advanced device designed to maintain target body temperatures with disposable gel pads and continuous core temperature monitoring.
Demographics and Challenges
Ultimately, with the majority of the study's participants being over 80% from Korea and a median age of 62 years, the research underscores the diverse challenges faced in cerebrovascular disease management. The lack of blinding in the trial may also have influenced treatment protocols, introducing further complexities to the outcomes.
Future Research Directions
While the INTREPID trial offers valuable insights into ICU fever management post-stroke, it also paves the way for more specialized and nuanced studies that seek to find effective solutions for specific patient groups. As the medical community grapples with these findings, the quest to find an effective post-stroke management strategy continues.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)