Breakthrough Inhibitor Could Turn the Tide Against Flesh-Eating Bacteria!
2025-03-17
Author: Sarah
Introduction
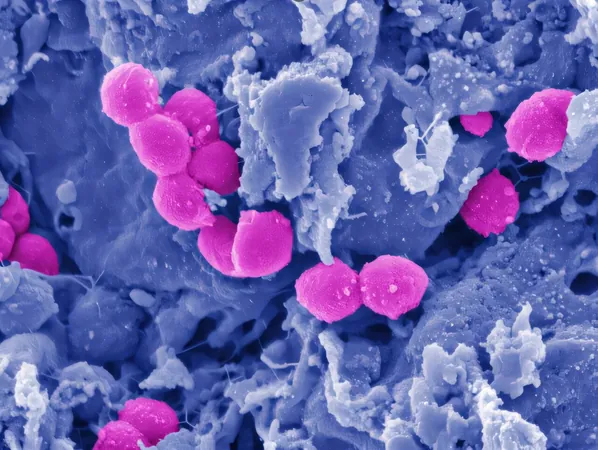
In a groundbreaking study published in *Nature Communications*, researchers have unveiled an innovative method to combat the ravaging effects of *Streptococcus pyogenes*, the notorious flesh-eating bacterium linked to deadly conditions such as necrotizing fasciitis. The research emphasizes the game-changing potential of disrupting bacterial metabolism to minimize tissue damage during severe infections, paving the way for improved healing processes.
Research Collaboration
Led by Dr. Wei Xu, an assistant professor of biomedical sciences at the Marshall University Joan C. Edwards School of Medicine, this collaboration also draws insights from Washington University School of Medicine and Central China Normal University. The team’s investigation focused on how *S. pyogenes* cleverly hijacks the host’s immune response through its unique aerobic mixed-acid fermentation process. This mechanism generates harmful metabolic byproducts, specifically acetate and formate, which significantly impair immune cell functionality, delay the elimination of the bacteria, and hinder wound recovery.
The Breakthrough Discovery
Remarkably, by utilizing a pyruvate dehydrogenase inhibitor to target and interrupt this bacterial metabolic strategy, the researchers demonstrated a significant reduction in tissue damage in a mouse model suffering from necrotizing skin infections. This groundbreaking discovery opens up a fresh avenue for therapeutic intervention—a method that could not only bolster the body’s tolerance to infection but also serve as an advantageous supplement to existing antibiotic treatments.
Implications for the Medical Community
In a time when antibiotic resistance is a growing concern and complications such as excessive inflammation can worsen patient conditions, this new approach holds great promise. Dr. Xu stated, "This study sheds light on how bacterial metabolism influences the immune system. By understanding these interactions, we are poised to devise new treatment strategies that not only protect tissues but also enhance the effectiveness of antibiotics, ultimately improving patient outcomes."
Conclusion
As the medical community races against time to find effective solutions to combat severe bacterial infections, this research highlights the critical need to rethink traditional treatment strategies. The potential to harness reprogrammed bacterial metabolism not only raises hopes for new therapies but also signifies a dramatic shift in how we understand the relationship between bacteria and host responses. Stay tuned for further updates on this pivotal research that could redefine treatment for life-threatening infections!
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)