Breakthrough in Schizophrenia Treatment: Transcranial Magnetic Stimulation Shows Promise Against Auditory Hallucinations
2024-11-13
Author: Yu
Introduction
In an exciting development for mental health treatment, researchers at Anhui Medical University in China have demonstrated that auditory verbal hallucinations (AVH) in schizophrenia patients can be significantly alleviated through magnetic resonance imaging (MRI)-guided repetitive transcranial magnetic stimulation (rTMS). This groundbreaking study, recently published in JAMA Network Open, involved a rigorous six-week, double-blind, sham-controlled trial with 62 participants.
About Auditory Verbal Hallucinations
Auditory verbal hallucinations, characterized by individuals hearing voices that do not exist, affect around 75% of those diagnosed with schizophrenia at the onset. Alarmingly, up to 30% of patients continue to experience these distressing symptoms even after undergoing standard antipsychotic treatments. Such persistent hallucinations not only diminish the quality of life but also elevate the risk of suicidal ideation and violent behavior, highlighting an urgent need for innovative therapeutic solutions.
Study Overview
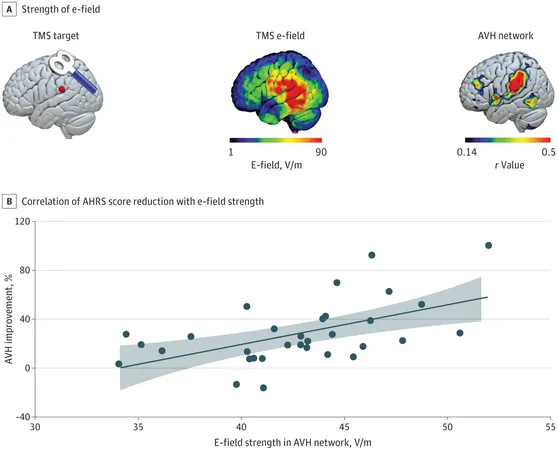
The clinical trial focused on assessing the effects of MRI-navigated rTMS on AVH, with particular attention to its ability to target the left temporoparietal junction—a crucial brain area implicated in the generation of these hallucinations. Unlike traditional methods that employ the international 10-20 system for TMS coil placement, the MRI-navigated approach allows for more precision in targeting problematic brain regions.
Methodology
Participants were randomized to receive either active rTMS or a sham treatment over a two-week period, with assessments made using the Auditory Hallucination Rating Scale (AHRS) at baseline, at the end of the treatment, and in a follow-up six weeks later. The results were promising; those receiving active rTMS reported a substantial reduction in their AHRS scores—an average decrease of 26.8% by week two compared to just 4.4% in the sham group. This effect was not ephemeral; at week six, the active rTMS group demonstrated an even more impressive average decrease of 33.3%.
Results and Implications
Moreover, a correlation was found linking stronger TMS-induced electric fields within the targeted brain network to greater reductions in AVH severity. Notably, this enhancement did not stem from increased output from the rTMS equipment but rather from the unique neuroanatomical features of the individual participants, allowing for tailored treatments.
Safety Profile
Importantly, no serious adverse effects were reported throughout the trial, suggesting that MRI-guided rTMS is not only effective but also a safe alternative treatment for AVH in schizophrenia.
Conclusion and Future Directions
While these findings are promising, the researchers emphasized the necessity for larger multisite trials to validate their results and further investigate how various clinical factors might influence treatment efficacy. As we await further research in this area, this study represents a significant leap forward in addressing one of the most challenging aspects of schizophrenia care.
Final Thoughts
Stay tuned—this could revolutionize how we tackle auditory hallucinations for millions suffering around the globe!
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)