Breakthrough in Battling 'Zombie' Tuberculosis Cells: New Drug Strategies Unveiled
2025-07-03
Author: Ming
Exciting advancements in tuberculosis (TB) research are paving the way for new treatments targeting the notorious 'zombie' cells of this deadly disease. A groundbreaking study from the University of Surrey, recently published in Scientific Reports, reveals a major leap in our fight against these elusive bacteria.
Known as 'persister cells,' these dormant, drug-tolerant TB bacteria can withstand even the harshest antibiotic treatments by entering a state of dormancy. When treatments are halted, they can reactivate, leading to relapses and persistent infections that challenge public health.
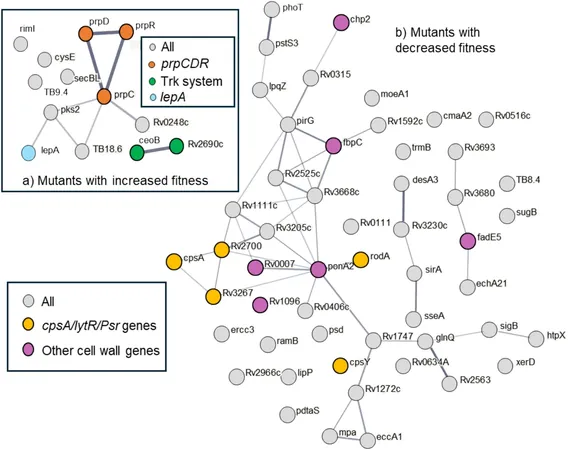
Current treatment methods demand prolonged multi-drug therapies that often fail, contributing to the alarming rise of antimicrobial resistance (AMR). To tackle this, the Surrey team examined a staggering library of over 500,000 genetically modified TB bacteria, exposing them to two common antibiotics: rifampicin and streptomycin. This rigorous selection process allowed them to identify those genes crucial for the survival of these zombie cells.
The researchers discovered that certain genes, when disrupted, significantly decreased the number of surviving persister cells. These genes play various roles, including weakening the bacterial cell wall, initiating a self-destruction process within the bacteria, and disrupting the cell’s metabolic functions. Each pathway presents a new avenue to develop revolutionary drugs aimed at swiftly eliminating these resilient pathogens.
Dr. Suzie Hingley-Wilson, co-author of the study and Senior Lecturer in Bacteriology, emphasized the urgency of addressing the TB crisis, which resulted in 1.3 million deaths last year, primarily due to drug-sensitive strains. "It's not just about antibiotic resistance; persister cells pose a significant hurdle. This research highlights that the survival of these cells is dependent on the specific antibiotics used, which reshapes our approach to TB treatment design,” she noted.
Moreover, mutations in some of the identified genes correspond to TB strains found in patients resistant to treatment, indicating that the lab findings could reflect real-world challenges faced in treating infections. This correlation is vital for understanding why certain patients experience treatment failures despite having non-resistant bacterial strains.
Professor Johnjoe McFadden, the study’s lead, stated, "The mechanisms behind bacterial persistence are some of microbiology's greatest mysteries. Solving them could transform how we tackle difficult diseases like TB. This research opens the door to new drugs specifically targeting persister cells, ultimately shortening treatment durations and easing the burden of AMR."
As the next phase of research begins, the scientific community holds great hope that these insights will pave the way for shorter, more effective treatments, significantly impacting global health efforts against tuberculosis.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)