Breakthrough in AML: MRD Testing Ramps Up Survival Rates for Young Patients
2025-05-05
Author: Mei
Revolutionary MRD Testing Improves Outcomes
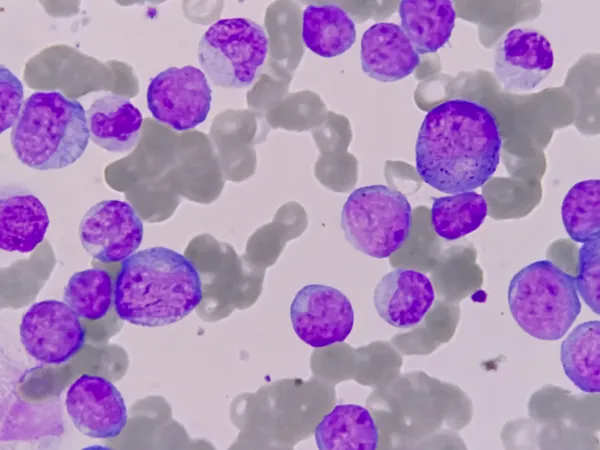
New research reveals that sequential measurable residual disease (MRD) testing dramatically enhances survival rates for younger patients battling acute myeloid leukemia (AML), particularly those with NPM1 and FLT3-ITD mutations. Published in The Lancet Haematology, this groundbreaking study could reshape future treatment protocols.
Significant Survival Benefits Revealed
Patients identified with both mutations who underwent MRD monitoring experienced an astounding 47% reduction in the risk of death, compared to those without monitoring. This innovative approach allows doctors to tailor treatments based on MRD findings, potentially revolutionizing care for this aggressive cancer.
Expert Insights on the Importance of Early Detection
Senior researcher Richard Dillon, FRCPath, from King’s College London, emphasizes the critical nature of early detection, stating, "AML is the most aggressive form of blood cancer. Identifying a patient's risk of relapse promptly is essential for effective treatment planning. We aspire to see these tests integrated into standard care, ultimately improving long-term survival rates for patients."
Study Design: Examining Real-World Impacts
The research examined participants across two UK trials (AML17 and AML19), focusing on those aged 16 to 60 newly diagnosed with AML. Patients were screened for specific molecular markers and randomly assigned to receive either MRD monitoring or standard care. The monitoring continued throughout treatment and for three years post-therapy.
Striking Results: A Closer Look
Though the overall survival rate was 70% for those monitored and 73% for those who weren’t, exciting insights emerged from subgroup analyses: patients with NPM1 and FLT3-ITD mutations recorded a three-year survival rate of 69% with MRD monitoring — a significant leap from 58% without it.
Hope for the Future of AML Treatment
Meanwhile, patients solely with NPM1 mutations showed a survival rate of 69% under monitoring, contrasted with 78% in the non-monitoring group. For those harboring fusion gene transcripts, the rates were 72% and 77% respectively. Co-author Nigel Russell, FRCPath, asserts, "There’s still so much to discover about treating this fast-evolving cancer. We hope our findings pave new pathways for relapse detection and offer renewed hope to those affected by AML."


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)